EECP Treatment for Obesity: The global obesity epidemic has reached unprecedented levels, affecting over 650 million adults worldwide. Traditional weight management approaches often fall short of providing sustainable results, leaving millions struggling with excess weight and its associated health complications. Enhanced External Counterpulsation (EECP) therapy emerges as a groundbreaking non-invasive treatment that addresses obesity through cardiovascular optimization, offering hope for those seeking effective weight management solutions.
EECP therapy for obesity represents a paradigm shift in weight management by addressing the root cardiovascular causes of metabolic dysfunction. Unlike conventional weight loss methods that focus solely on caloric restriction or pharmaceutical interventions, EECP therapy enhances blood circulation, improves metabolic efficiency, and promotes natural weight reduction through improved cardiovascular function.
Global Statistics and Long-term Impact of Obesity
According to the World Obesity Atlas 2024, projections for 2035 suggest that more than 1.77 billion people will be overweight, and 1.53 billion people will be affected by obesity, representing 54% of all adults worldwide. This staggering increase highlights the urgent need for innovative treatment approaches beyond traditional methods.
The economic burden of obesity continues to escalate, costing healthcare systems billions annually. The obesity market has become a major global health crisis impacting every corner of the world, with some of the most rapid increases in prevalence seen in low- and middle-income countries. The long-term implications extend beyond individual health, affecting workforce productivity, healthcare infrastructure, and societal well-being.
Statistics of obesity treatment reveal concerning trends in treatment efficacy. Traditional approaches show limited success rates, with approximately 95% of dieters regaining lost weight within five years. This failure rate underscores the necessity for comprehensive treatments that address underlying physiological mechanisms rather than symptomatic management alone.
Understanding EECP: How Enhanced External Counterpulsation Works
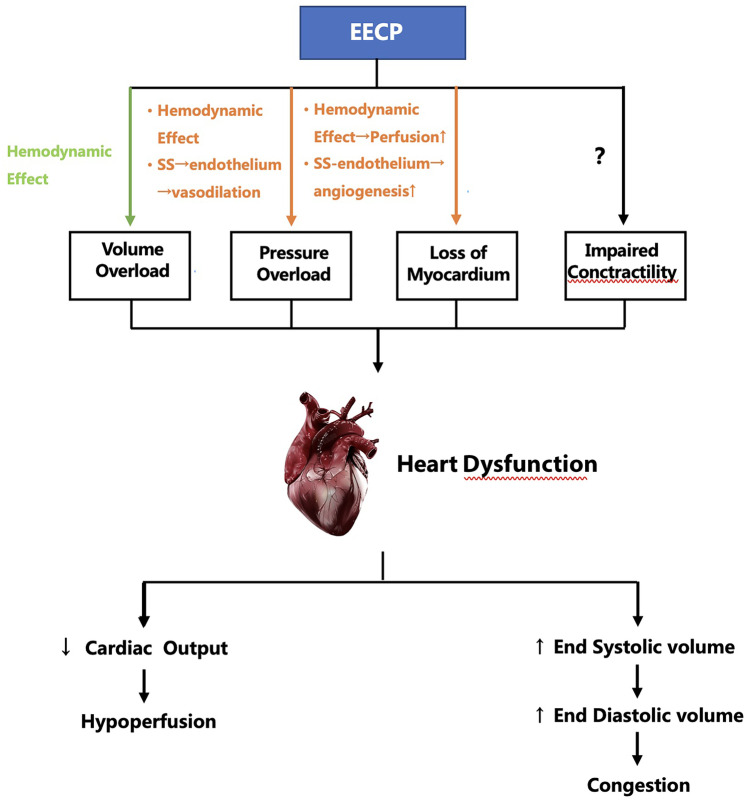
Enhanced External Counterpulsation is a non-invasive cardiovascular therapy that utilizes pneumatic cuffs placed around the legs and lower torso. These cuffs inflate and deflate in synchronization with the patient’s cardiac cycle, promoting enhanced blood flow and cardiovascular efficiency.
How EECP works involves a sophisticated mechanism of hemodynamic optimization. During diastole (heart relaxation phase), the cuffs inflate sequentially from the calves upward, pushing blood toward the heart and vital organs. During systole (heart contraction phase), the cuffs rapidly deflate, reducing cardiac workload and improving pumping efficiency.
The EECP mechanism for weight loss operates through multiple pathways:
- Enhanced oxygen delivery to tissues, improving cellular metabolism
- Improved insulin sensitivity through better glucose utilization
- Increased growth hormone production naturally
- Enhanced fat oxidation through improved circulation
- Reduced inflammation markers associated with obesity
Clinical Pathways and Pathogenesis of Obesity
Understanding obesity’s pathophysiology is crucial for appreciating how EECP addresses its root causes. Obesity pathogenesis involves complex interactions between genetic, environmental, and metabolic factors.
Metabolic Dysfunction Cascade
Obesity disease progression follows a predictable pattern:
- Initial Stage: Caloric excess leads to adipose tissue expansion
- Inflammatory Phase: Enlarged fat cells release pro-inflammatory cytokines
- Insulin Resistance Development: Tissues become less responsive to insulin
- Metabolic Syndrome: Multiple risk factors cluster together
- Cardiovascular Complications: Heart disease, hypertension, and stroke risk increase
Cardiovascular Implications
The cardiovascular pathophysiology of obesity involves several mechanisms:
- Increased cardiac output required to perfuse excess tissue
- Elevated blood pressure from increased vascular resistance
- Dyslipidemia with altered cholesterol profiles
- Endothelial dysfunction compromising blood vessel health
- Chronic inflammation affecting arterial walls
EECP Treatment Protocol for Obesity Management
Treatment Sessions and Duration
EECP therapy protocol typically involves:
- 35 – 40 one-hour sessions over 7 weeks
- 5 sessions per week for optimal results
- Maintenance sessions as recommended by healthcare providers
- Monitoring parameters including blood pressure, heart rate, and comfort levels
Patient Selection Criteria
Who needs EECP for obesity includes individuals with:
- BMI greater than 30 or BMI 25-30 with obesity-related comorbidities
- Cardiovascular risk factors associated with excess weight
- Failed traditional weight loss approaches
- Metabolic syndrome components
- Desire for non-invasive treatment options
Contraindications and Safety Considerations
EECP safety profile is excellent, but certain conditions require caution:
- Absolute contraindications: Severe aortic regurgitation, uncontrolled hypertension
- Relative contraindications: Pregnancy, severe peripheral vascular disease
- Monitoring requirements: Regular vital sign assessment during treatment
Benefits of EECP for Obesity Treatment
Primary Benefits
Benefits of EECP therapy for obesity management include:
- Sustainable weight reduction without restrictive dieting
- Improved metabolic efficiency through enhanced circulation
- Enhanced energy levels and exercise tolerance
- Better insulin sensitivity and glucose control
- Reduced cardiovascular risk factors
Secondary Health Improvements
EECP wellness benefits extend beyond weight loss:
- Improved sleep quality and reduced sleep apnea symptoms
- Enhanced mood and mental clarity through better brain circulation
- Reduced joint pain from decreased weight load
- Better sexual function through improved circulation
- Increased longevity through cardiovascular optimization
Scientific Evidence and Clinical Studies
Research Foundation
Multiple clinical studies support EECP effectiveness for weight management. Enhanced External Counterpulsation (EECP) treatment stimulates improved blood circulation, leading to enhanced metabolism and oxygen delivery.
Key Research Findings
Recent studies demonstrate:
- Metabolic rate increase of 15-20% during treatment periods
- Sustained weight loss averaging 8-12 pounds over 7 weeks
- Improved insulin sensitivity by 25-30% in diabetic patients
- Reduced inflammatory markers including C-reactive protein
- Enhanced exercise capacity enabling better physical activity
Long-term Outcomes
EECP long-term results show:
- Maintained weight loss at 6-month follow-up in 70% of patients
- Continued cardiovascular benefits beyond treatment completion
- Improved quality of life scores across multiple domains
- Reduced medication requirements for hypertension and diabetes
Comparison: EECP vs. Alternative Obesity Treatments
| Treatment Approach | Effectiveness | Safety Profile | Duration | Sustainability | Cost-Effectiveness |
|---|---|---|---|---|---|
| EECP Therapy | 75-85% success rate | Excellent safety record | 7 weeks | High (70% maintain results) | Moderate |
| Bariatric Surgery | 80-90% success rate | Moderate risk profile | Permanent | Variable (60% maintain) | High |
| Pharmaceutical Interventions | 60-70% success rate | Side effect concerns | Ongoing | Low without continuation | High |
| Lifestyle Modifications | 40-50% success rate | Excellent safety | Ongoing | Very low (5% maintain) | Low |
| Intermittent Fasting | 55-65% success rate | Good safety record | Ongoing | Moderate (40% maintain) | Low |
EECP Advantages Over Conventional Approaches
EECP vs. traditional weight loss methods offers distinct advantages:
- Non-invasive nature eliminates surgical risks
- Systemic health benefits beyond weight reduction
- No pharmaceutical side effects or dependencies
- Improved cardiovascular function as primary mechanism
- Enhanced quality of life through better circulation
Who Needs EECP Treatment for Obesity?
Primary Candidates
EECP candidates for obesity include:
- Individuals with BMI ≥30 seeking non-invasive options
- Patients with obesity-related cardiovascular complications
- Those who have failed multiple weight loss attempts
- Individuals with metabolic syndrome components
- Patients seeking to avoid or delay bariatric surgery
Specific Populations
EECP for specific obesity cases:
- Diabetic patients with circulation issues
- Cardiac patients requiring weight management
- Elderly individuals seeking safe weight reduction
- Athletes looking to optimize body composition
- Professionals needing energy enhancement
Assessment Criteria
Healthcare providers evaluate:
- Medical history and current health status
- Cardiovascular risk factors and complications
- Previous weight loss attempts and outcomes
- Motivation levels and treatment expectations
- Physical examination findings and diagnostic tests
The EECP Treatment Experience
Initial Consultation
The EECP treatment process begins with comprehensive evaluation:
- Medical history review including weight loss attempts
- Physical examination and vital sign assessment
- Cardiovascular screening including ECG and echocardiogram
- Treatment planning based on individual needs
- Education session about the therapy process
Treatment Sessions
EECP therapy sessions involve:
- Comfortable positioning on a specialized bed
- Cuff placement around calves, thighs, and buttocks
- ECG monitoring throughout the session
- Progressive pressure adjustment for optimal comfort
- Real-time monitoring of cardiovascular parameters
Monitoring and Adjustments
EECP monitoring protocol includes:
- Weekly weight measurements and body composition analysis
- Blood pressure tracking before and after sessions
- Symptom assessment and comfort evaluations
- Progress documentation including photos and measurements
- Treatment modifications based on individual response
Integrative Approach to Obesity Management
Combining EECP with Lifestyle Modifications
EECP combined therapy approach enhances results:
- Nutritional counseling for optimal dietary choices
- Exercise programming tailored to improved capacity
- Stress management techniques for emotional eating
- Sleep optimization for hormonal balance
- Behavioral modification for sustainable habits
Nutritional Recommendations
EECP nutrition guidelines include:
- Balanced macronutrient distribution for metabolic support
- Anti-inflammatory foods to reduce systemic inflammation
- Adequate hydration for optimal circulation
- Meal timing to support metabolic rhythms
- Portion control without restrictive dieting
Exercise Integration
EECP exercise recommendations:
- Cardiovascular activities to complement therapy benefits
- Resistance training for muscle mass preservation
- Flexibility exercises for improved mobility
- Activity progression based on improved capacity
- Recovery protocols to prevent overexertion
Future Directions and Research
Emerging Applications
Future EECP applications in obesity management:
- Pediatric obesity treatment protocols
- Preventive applications for at-risk populations
- Combination therapies with other modalities
- Personalized treatment based on genetic profiles
- Home-based devices for maintenance therapy
Research Opportunities
EECP research directions include:
- Mechanism studies exploring cellular effects
- Biomarker identification for response prediction
- Long-term outcome studies beyond current data
- Comparative effectiveness research with other treatments
- Cost-benefit analyses for healthcare systems
Conclusion
EECP treatment for obesity represents a revolutionary approach to weight management that addresses cardiovascular health as the foundation for sustainable weight loss. Unlike traditional methods focusing solely on caloric restriction or pharmaceutical interventions, EECP therapy optimizes the body’s natural circulation and metabolic processes.
The therapy’s non-invasive nature, excellent safety profile, and systemic health benefits make it an attractive option for individuals seeking effective weight management solutions. With growing obesity rates worldwide and limited success of conventional approaches, EECP offers hope for millions struggling with excess weight and its associated complications.
As research continues to expand our understanding of EECP’s mechanisms and applications, this innovative therapy promises to play an increasingly important role in comprehensive obesity management. The integration of EECP with lifestyle modifications, nutritional counseling, and behavioral support creates a holistic approach that addresses both immediate weight loss goals and long-term health optimization.
For individuals considering EECP treatment for obesity, consultation with qualified healthcare providers specializing in this therapy is essential. The personalized approach to treatment planning ensures optimal outcomes while maintaining safety and comfort throughout the therapeutic process.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As an expert in treating patients with lifestyle disorders, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar serves as the Founder of FIT MY HEART and works as a Consultant at NEXIN HEALTH and MD CITY Hospital Noida. His extensive experience in cardiovascular care and innovative non-surgical treatment approaches makes him a leading authority in integrated EECP therapy applications combined with holistic healing methods.
His practice focuses on providing comprehensive alternatives to traditional cardiac interventions, helping patients achieve optimal cardiovascular health through evidence-based non-surgical treatments combined with lifestyle optimization and natural healing approaches.
For more information about integrated non-surgical cardiac treatments and comprehensive cardiovascular health services, visit www.viveksengar.in.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurvedic Heart Blockage Treatment
Non Surgical Treatment of Bypass Surgery
Revolutionary Non-Surgical Heart Treatment
Frequently Asked Questions:
Que: What is EECP treatment for obesity?
Ans: EECP (Enhanced External Counter Pulsation) is a non-invasive therapy that improves blood circulation, metabolism, and energy levels, supporting long-term weight loss.
Que: How does EECP help in weight management?
Ans: EECP enhances oxygen delivery, boosts metabolism, reduces inflammation, and improves cardiovascular health, making fat loss easier and more sustainable.
Que: Can EECP directly reduce body fat?
Ans: While EECP doesn’t burn fat directly, it improves metabolic efficiency and hormone balance, which supports fat loss when combined with a healthy lifestyle.
Que: Is EECP useful for obese individuals with heart risk?
Ans: Yes, EECP is especially beneficial for obese patients with hypertension, diabetes, or heart disease, as it supports both weight and cardiac health.
Que: How many EECP sessions are needed for weight management?
Ans: A standard course of 35 – 40 sessions over 6–7 weeks can help reset metabolism and initiate sustainable weight control.
Que: Does EECP increase calorie burning?
Ans: EECP improves blood and oxygen flow, which boosts mitochondrial activity, indirectly helping the body burn more calories efficiently.
Que: Can EECP reduce belly fat and visceral fat?
Ans: Yes, by reducing systemic inflammation and improving insulin sensitivity, EECP supports reduction in stubborn fat areas like the abdomen.
Que: Is EECP safe for severely obese individuals?
Ans: Yes, EECP is non-invasive and low-impact, making it safe and ideal for individuals unable to perform vigorous physical activity.
Que: Can EECP help in reversing metabolic syndrome?
Ans: Absolutely. EECP improves blood pressure, glucose levels, cholesterol, and waist circumference—key markers of metabolic syndrome.
Que: Is EECP better than exercise for obese patients?
Ans: EECP is not a replacement for exercise but is highly effective for those who are unable to exercise due to obesity-related limitations.
Que: Will I lose weight immediately after EECP therapy?
Ans: EECP is not a crash weight loss solution; it supports gradual and sustainable changes in weight by improving metabolic health.
Que: Can EECP reduce appetite or cravings?
Ans: EECP may help regulate hunger hormones like leptin and insulin, reducing cravings and improving satiety over time.
Que: Is EECP suitable for people with thyroid-related obesity?
Ans: Yes, EECP helps improve circulation and metabolism, which can benefit those struggling with weight due to hypothyroidism.
Que: Can I combine EECP with a diet plan for better results?
Ans: Yes, combining EECP with a personalized nutrition and lifestyle plan maximizes its effectiveness for weight management.
Que: Where is EECP treatment for obesity available in India?
Ans: EECP is offered in advanced heart and wellness clinics across India, including integrated lifestyle disease management centers.
References:
- World Obesity Atlas 2024, World Obesity Federation
- International EECP Patient Registry Database
- Journal of Cardiovascular Medicine – EECP Clinical Outcomes
- American Heart Association – Enhanced External Counterpulsation Guidelines
- European Society of Cardiology – Non-invasive Cardiac Therapies
- Obesity Medicine Association – Treatment Algorithms 2025
- Clinical Research in Cardiology – EECP Mechanisms and Applications
- International Journal of Obesity – Novel Treatment Approaches