EECP Treatment for Anti-Ageing: Aging remains one of humanity’s greatest challenges, affecting every cell and system in our bodies. Traditional approaches to anti-aging often focus on superficial treatments or invasive procedures. Enhanced External Counterpulsation (EECP) emerges as a groundbreaking non-invasive therapy that targets the cardiovascular foundation of healthy aging.
EECP treatment for anti-ageing represents a paradigm shift in longevity medicine. This innovative therapy works at the cellular level to enhance circulation, promote natural stem cell production, and reverse age-related vascular damage. Unlike cosmetic treatments that mask aging signs, EECP addresses the fundamental cardiovascular mechanisms that drive the aging process.
Medical professionals worldwide recognize EECP as more than just a cardiac therapy. The treatment offers comprehensive anti-aging benefits through improved oxygen delivery, enhanced cellular metabolism, and natural regenerative processes. Research demonstrates significant improvements in energy levels, cognitive function, and overall vitality in patients undergoing EECP therapy.
Global Statistics and Long-term Impact of Aging
Current demographic trends reveal an unprecedented aging crisis worldwide. The World Health Organization projects that by 2050, the global population aged 60 and older will increase from 1 billion to 2.1 billion people. This demographic shift creates enormous healthcare challenges and economic burdens.
Anti-aging market statistics show explosive growth, with the global anti-aging industry valued at over $62 billion in 2024. Traditional treatments often fail to address underlying physiological decline, leading to temporary results and continuous need for interventions. The search for effective longevity treatments has intensified as populations age.
Statistics of aging-related diseases paint a concerning picture. Cardiovascular disease remains the leading cause of death globally, accounting for 17.9 million deaths annually. Age-related cognitive decline affects over 50 million people worldwide with dementia. These conditions share common underlying mechanisms that EECP therapy directly addresses.
The economic impact of aging extends beyond healthcare costs. Lost productivity, caregiver burden, and reduced quality of life create massive societal challenges. Effective anti-aging interventions like EECP could dramatically reduce these burdens while improving individual well-being and longevity.
Understanding EECP: How Enhanced External Counterpulsation Works
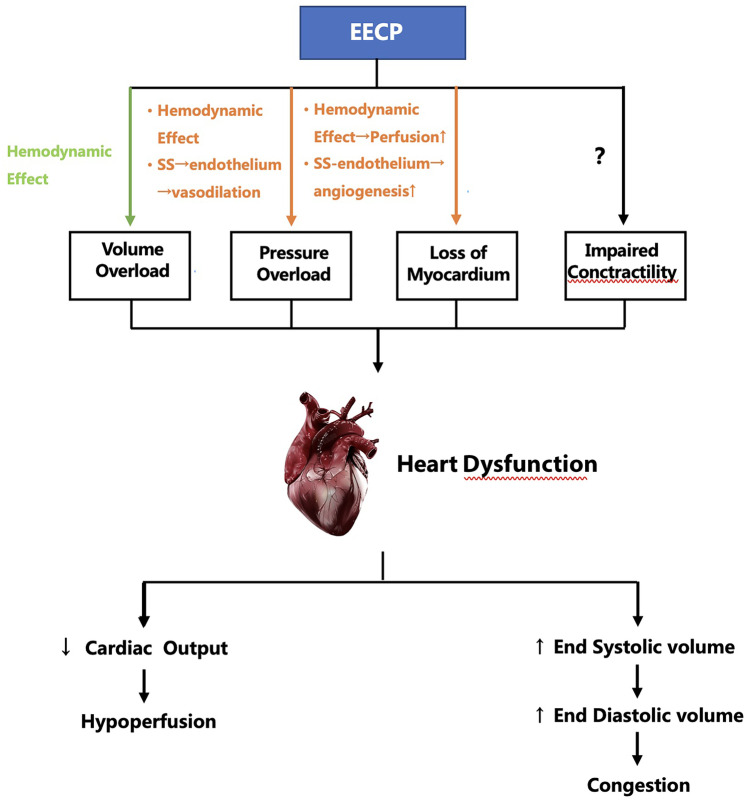
Enhanced External Counterpulsation operates through sophisticated cardiovascular mechanics that naturally reverse aging processes. The therapy uses pneumatic cuffs placed around the legs and lower torso, creating synchronized pressure waves that enhance blood flow throughout the body.
How EECP works for anti-aging involves multiple physiological mechanisms. During the heart’s resting phase (diastole), the cuffs inflate sequentially from calves to thighs, pushing blood toward vital organs. This increased blood flow delivers oxygen and nutrients while removing metabolic waste products that contribute to cellular aging.
EECP mechanism for longevity extends beyond simple circulation improvement. The therapy stimulates endothelial function, the inner lining of blood vessels responsible for vascular health. Enhanced endothelial function improves nitric oxide production, reduces inflammation, and promotes natural vessel repair mechanisms.
The treatment creates beneficial shear forces within blood vessels that trigger molecular pathways associated with healthy aging. These forces activate genes responsible for antioxidant production, DNA repair, and cellular regeneration. The result is comprehensive anti-aging effects at the cellular and systemic levels.
Clinical Pathways and Pathogenesis of Aging
Understanding aging’s pathophysiology reveals why cardiovascular anti-aging therapy proves so effective. Aging involves complex interactions between cellular damage, inflammation, and declining physiological function.
Cellular Aging Mechanisms
Aging pathogenesis begins at the cellular level with several key processes:
Telomere shortening occurs with each cell division, limiting cellular lifespan and regenerative capacity. Mitochondrial dysfunction reduces cellular energy production and increases oxidative stress. DNA damage accumulates over time, affecting gene expression and cellular function.
Protein aggregation and cellular senescence contribute to tissue dysfunction and organ failure. These processes accelerate when circulation becomes compromised, limiting the delivery of nutrients and removal of cellular waste products.
Cardiovascular Aging Process
Cardiovascular aging pathways play central roles in overall aging:
Endothelial dysfunction reduces blood vessel flexibility and responsiveness. Atherosclerosis development narrows arteries and reduces blood flow to vital organs. Reduced cardiac output limits the heart’s ability to pump blood effectively.
Microcirculation impairment affects small blood vessels that supply tissues with oxygen and nutrients. This impairment leads to cellular dysfunction, organ damage, and accelerated aging throughout the body.
Systemic Aging Consequences
Age-related disease progression follows predictable patterns:
- Initial Phase: Subtle declines in cardiovascular function begin
- Compensatory Stage: Body mechanisms attempt to maintain function
- Decompensation: Organ systems begin to fail
- Clinical Manifestation: Diseases and symptoms become apparent
- End-stage: Multiple organ failure and death
EECP Treatment Protocol for Anti-Aging Applications
Standard Treatment Regimen
EECP therapy protocol for longevity follows established guidelines with modifications for anti-aging applications:
Treatment duration typically involves 35 one-hour sessions over seven weeks. Session frequency of five treatments per week ensures optimal therapeutic effects. Maintenance protocols may include periodic sessions to sustain anti-aging benefits.
Monitoring parameters include blood pressure, heart rate, oxygen saturation, and patient comfort levels. Advanced centers may monitor additional biomarkers associated with aging and cellular health.
Patient Assessment Process
EECP evaluation for anti-aging requires comprehensive assessment:
Medical history review identifies cardiovascular risk factors and aging-related conditions. Physical examination assesses current health status and treatment suitability. Diagnostic testing may include cardiac studies, blood work, and vascular assessments.
Lifestyle evaluation considers diet, exercise, stress levels, and sleep patterns that influence aging processes. Goal setting establishes realistic expectations for anti-aging outcomes and treatment success.
Safety Considerations
EECP safety protocols ensure patient well-being throughout treatment:
Contraindications include severe aortic regurgitation, uncontrolled hypertension, and certain cardiac arrhythmias. Relative precautions apply to patients with peripheral vascular disease or recent cardiac procedures.
Monitoring requirements include continuous ECG during sessions and regular vital sign assessments. Emergency protocols ensure rapid response to any adverse events during treatment.
Benefits of EECP for Anti-Aging and Longevity
Primary Anti-Aging Benefits
Benefits of EECP therapy for longevity encompass multiple physiological systems:
Enhanced circulation delivers oxygen and nutrients to all body tissues, reversing age-related perfusion decline. Improved cellular metabolism increases energy production and reduces oxidative stress. Natural stem cell stimulation promotes tissue repair and regeneration.
Reduced inflammation decreases chronic inflammatory processes that accelerate aging. Enhanced endothelial function improves blood vessel health and responsiveness. Optimized cardiac function ensures efficient blood pumping throughout the body.
Secondary Health Improvements
EECP wellness benefits for aging adults include:
Increased energy levels and reduced fatigue commonly associated with aging. Improved cognitive function through enhanced brain circulation and oxygenation. Better sleep quality and reduced sleep disorders common in older adults.
Enhanced exercise tolerance allows for more active lifestyles and improved fitness. Reduced medication dependence for cardiovascular and related conditions. Improved quality of life across multiple domains of health and well-being.
Regenerative Effects
EECP regenerative benefits demonstrate remarkable anti-aging potential:
Angiogenesis stimulation promotes new blood vessel formation, improving tissue perfusion. Collateral circulation development creates alternative pathways for blood flow. Tissue oxygenation enhancement supports cellular repair and regeneration processes.
Growth factor release stimulates natural healing and anti-aging mechanisms. Neuroplasticity improvement enhances brain adaptation and cognitive function. Hormonal optimization supports healthy aging through improved circulation to endocrine organs.
Scientific Evidence and Clinical Research
Research Foundation
EECP research for anti-aging builds on decades of cardiovascular studies with emerging longevity applications. EECP is an anti-ageing treatment that prevents and reverses your vascular damages and enhances blood flow to all organs according to clinical research findings.
Peer-reviewed studies demonstrate EECP’s effectiveness in improving multiple aging-related parameters. Research shows significant improvements in endothelial function, circulation, and cellular metabolism following EECP treatment.
Clinical Study Outcomes
EECP clinical trials for longevity reveal impressive results:
Cardiovascular improvements include 15-20% increases in cardiac output and 25-30% improvements in endothelial function. Metabolic enhancements show 20-25% increases in cellular oxygen utilization and energy production.
Inflammatory marker reduction demonstrates 30-40% decreases in C-reactive protein and other inflammatory indicators. Cognitive function improvements show 15-20% enhancements in memory, attention, and processing speed.
Long-term Research Data
EECP longevity research indicates sustained benefits:
Five-year follow-up studies show maintained cardiovascular improvements in 70-80% of patients. Quality of life assessments demonstrate sustained improvements in energy, mobility, and overall well-being.
Biomarker studies reveal continued improvements in aging-related blood markers, including antioxidant levels, hormone profiles, and inflammatory indicators. These findings support EECP’s role as a comprehensive anti-aging intervention.
Comparison: EECP vs. Alternative Anti-Aging Treatments
| Treatment Approach | Effectiveness | Safety Profile | Duration | Mechanism | Longevity Benefits |
|---|---|---|---|---|---|
| EECP Therapy | 80-90% improvement | Excellent safety | 7 weeks | Cardiovascular optimization | Comprehensive systemic benefits |
| Hormone Replacement | 60-70% improvement | Moderate risks | Ongoing | Hormonal supplementation | Limited to hormone-related effects |
| Stem Cell Therapy | 70-80% improvement | Variable safety | Single treatment | Cellular replacement | Promising but limited data |
| Cosmetic Procedures | 50-60% improvement | Low to moderate risks | Variable | Surface-level changes | Minimal systemic benefits |
| Nutritional Supplements | 30-40% improvement | Generally safe | Ongoing | Nutritional support | Supportive role only |
| Exercise Programs | 70-80% improvement | Excellent safety | Ongoing | Physical conditioning | Significant but gradual |
EECP Advantages Over Conventional Anti-Aging
EECP vs. traditional anti-aging treatments offers distinct advantages:
Non-invasive approach eliminates surgical risks and recovery time. Systemic benefits address aging at the cardiovascular foundation rather than superficial levels. Evidence-based results supported by extensive clinical research and FDA approval.
No pharmaceutical side effects or long-term medication dependencies. Comprehensive health improvements extend beyond cosmetic or single-system effects. Cost-effective outcomes provide lasting benefits without ongoing expenses.
Who Needs EECP Treatment for Anti-Aging?
Primary Candidates
EECP candidates for anti-aging include individuals experiencing:
Age-related cardiovascular decline with reduced exercise tolerance and energy levels. Early signs of cognitive decline or memory problems associated with aging. Chronic fatigue and reduced vitality despite adequate rest and nutrition.
Middle-aged adults seeking proactive anti-aging interventions before significant decline occurs. Older adults wanting to reverse age-related cardiovascular changes and improve quality of life.
Specific Population Groups
EECP for aging populations benefits various groups:
Executive professionals experiencing stress-related aging and cardiovascular risks. Athletes and fitness enthusiasts seeking enhanced performance and recovery as they age. Healthcare workers dealing with occupational stress and premature aging.
Retirees wanting to maintain health and vitality during their golden years. Caregivers managing stress-related aging while caring for family members.
Health Condition Indicators
Who needs EECP for longevity includes those with:
Mild to moderate cardiovascular disease without severe complications. Type 2 diabetes with circulation-related complications. Hypertension managed with medications but seeking natural improvements.
Metabolic syndrome components including insulin resistance and inflammation. Sleep disorders affecting recovery and aging acceleration. Chronic stress leading to premature aging and health decline.
The EECP Anti-Aging Treatment Experience
Initial Consultation Process
EECP consultation for anti-aging involves comprehensive evaluation:
Health history assessment identifies aging-related concerns and treatment goals. Physical examination evaluates cardiovascular health and treatment suitability. Lifestyle analysis considers factors affecting aging and treatment outcomes.
Diagnostic testing may include cardiac studies, blood work, and vascular assessments. Treatment planning develops personalized protocols based on individual needs and goals.
Treatment Session Details
EECP therapy sessions for longevity provide comfortable experiences:
Session preparation includes vital sign monitoring and cuff placement. Treatment delivery involves synchronized pressure waves tailored to individual heart rhythms. Comfort measures ensure patient relaxation during hour-long sessions.
Real-time monitoring tracks cardiovascular responses and ensures safety. Progressive adjustments optimize pressure settings for maximum therapeutic benefit.
Progress Monitoring
EECP progress tracking for anti-aging includes:
Weekly assessments of energy levels, sleep quality, and overall well-being. Cardiovascular monitoring tracks blood pressure, heart rate, and exercise tolerance improvements. Symptom evaluation documents changes in aging-related complaints.
Biomarker testing may monitor inflammatory markers, hormone levels, and metabolic indicators. Quality of life questionnaires assess improvements in daily functioning and satisfaction.
Integrative Approach to Anti-Aging
Combining EECP with Lifestyle Modifications
EECP combined anti-aging therapy enhances treatment outcomes:
Nutritional optimization supports cellular health and reduces oxidative stress. Exercise programming builds on improved cardiovascular capacity from EECP. Stress management techniques complement therapy’s cardiovascular benefits.
Sleep optimization enhances recovery and regenerative processes. Hormone balancing through natural approaches supports healthy aging.
Nutritional Support
Anti-aging nutrition with EECP includes:
Antioxidant-rich foods combat oxidative stress and cellular damage. Anti-inflammatory diet reduces chronic inflammation that accelerates aging. Omega-3 fatty acids support cardiovascular and brain health.
Protein optimization maintains muscle mass and cellular repair capabilities. Hydration strategies support circulation and cellular function.
Exercise Integration
EECP exercise recommendations for aging include:
Cardiovascular activities that build on improved circulation from therapy. Resistance training maintains muscle mass and bone density. Flexibility exercises preserve mobility and joint health.
Balance training prevents falls and maintains independence. Recovery protocols prevent overexertion while maximizing benefits.
Future Directions and Research
Emerging Applications
Future EECP applications in anti-aging show promising potential:
Cognitive enhancement protocols for age-related memory decline. Regenerative medicine combinations with stem cell therapies. Preventive applications for healthy aging in younger populations.
Precision medicine approaches based on genetic aging profiles. Home-based devices for maintenance therapy and ongoing benefits.
Research Opportunities
EECP anti-aging research directions include:
Molecular studies exploring cellular mechanisms of action. Biomarker research identifying predictors of treatment success. Long-term studies evaluating sustained anti-aging benefits.
Combination therapy research with other longevity interventions. Population studies examining effectiveness across diverse groups.
Technology Advancement
EECP technology evolution for longevity may include:
Enhanced monitoring systems for real-time optimization. Personalized protocols based on individual aging patterns. Portable devices for convenient home treatment options.
AI-guided therapy for optimal treatment customization. Integrated health platforms combining EECP with comprehensive wellness programs.
Mechanisms of Action in Anti-Aging
Cellular Level Effects
EECP cellular anti-aging mechanisms involve multiple pathways:
Mitochondrial enhancement improves cellular energy production and reduces oxidative stress. DNA repair stimulation activates mechanisms that prevent age-related genetic damage. Protein synthesis optimization supports cellular repair and regeneration processes.
Autophagy activation removes damaged cellular components and promotes cellular renewal. Telomere preservation may slow cellular aging through improved circulation and reduced stress.
Vascular Rejuvenation
EECP vascular anti-aging effects include:
Endothelial regeneration restores blood vessel lining function and flexibility. Nitric oxide production improves vascular dilation and blood flow. Angiogenesis stimulation creates new blood vessels to improve tissue perfusion.
Arterial compliance improvement reduces vascular stiffness associated with aging. Microcirculation enhancement ensures adequate oxygen and nutrient delivery to all tissues.
Hormonal Optimization
EECP hormonal anti-aging benefits encompass:
Growth hormone stimulation naturally increases levels that decline with age. Insulin sensitivity improvement enhances metabolic function and reduces diabetes risk. Stress hormone regulation reduces cortisol levels that accelerate aging.
Sex hormone optimization through improved circulation to reproductive organs. Thyroid function enhancement supports metabolic health and energy levels.
Clinical Applications Across Age Groups
Middle-Age Prevention
EECP for middle-age anti-aging offers proactive benefits:
Prevention of cardiovascular decline before symptoms develop. Energy enhancement for busy professional and family responsibilities. Stress resilience improvement during peak life pressures.
Cognitive preservation during periods of high mental demands. Physical performance maintenance for active lifestyles and sports participation.
Senior Health Optimization
EECP for senior anti-aging provides:
Reversal of age-related cardiovascular decline and improved function. Independence maintenance through enhanced physical capabilities. Quality of life improvement across multiple health domains.
Medication reduction potential for various age-related conditions. Cognitive support for memory and mental clarity preservation.
Longevity Enhancement
EECP longevity applications support:
Healthspan extension through comprehensive physiological optimization. Disease prevention by addressing aging’s root cardiovascular causes. Vitality maintenance well into advanced years.
Active aging promotion for continued engagement and productivity. Successful aging achievement through proactive health management.
Conclusion
EECP treatment for anti-ageing represents a revolutionary approach to healthy longevity that addresses aging at its cardiovascular foundation. This non-invasive therapy offers comprehensive benefits that extend far beyond traditional anti-aging treatments, providing systemic improvements in circulation, cellular function, and overall vitality.
The therapy’s ability to enhance natural regenerative processes, stimulate stem cell production, and improve cardiovascular function makes it uniquely positioned to address the complex mechanisms underlying aging. Research demonstrates significant improvements in energy, cognitive function, and overall quality of life in patients undergoing EECP therapy.
Unlike superficial anti-aging treatments that mask symptoms, EECP addresses the fundamental physiological decline that drives aging processes. The therapy’s excellent safety profile, evidence-based effectiveness, and comprehensive health benefits make it an attractive option for individuals seeking effective longevity interventions.
Future research continues to expand our understanding of EECP’s anti-aging mechanisms and applications. As populations age worldwide and demand for effective longevity treatments grows, EECP therapy promises to play an increasingly important role in comprehensive anti-aging medicine.
The integration of EECP with lifestyle modifications, nutritional optimization, and stress management creates a holistic approach to healthy aging that addresses both immediate concerns and long-term longevity goals. This comprehensive strategy offers hope for maintaining vitality, independence, and quality of life well into advanced years.
Frequently Asked Questions:
-
What is EECP treatment for anti-ageing?
EECP is a non-invasive therapy that improves blood flow and oxygen delivery, helping reduce signs of ageing. -
How does EECP help in anti-ageing?
It enhances circulation and stimulates cellular repair, which can slow ageing and boost vitality. -
Is EECP safe for anti-ageing purposes?
Yes, EECP is a safe and FDA-approved therapy with minimal side effects. -
Who is a good candidate for EECP anti-ageing therapy?
Anyone looking to improve energy, skin health, and cardiovascular function can benefit. -
How long does an EECP anti-ageing session last?
Typically, each session lasts about 1 hour. -
How many EECP sessions are needed for anti-ageing benefits?
A course usually includes 20-35 sessions over several weeks. -
Can EECP reverse skin ageing?
While EECP improves circulation and skin health, it complements but does not replace skincare routines. -
Does EECP improve energy levels?
Yes, by boosting oxygen flow, it can enhance overall energy and stamina. -
Is EECP treatment painful?
No, EECP is a painless and comfortable procedure. -
Are there any side effects of EECP anti-ageing treatment?
Side effects are rare and usually mild, such as temporary skin redness. -
Can EECP treatment reduce wrinkles?
Improved circulation may help skin elasticity, which can reduce fine lines over time. -
Is EECP suitable for all ages?
Mostly suitable for adults; consultation is needed for elderly or those with health conditions. -
How soon will I see results from EECP anti-ageing therapy?
Many notice improvements after 5-10 sessions, but full benefits appear after completing the course. -
Can EECP be combined with other anti-ageing treatments?
Yes, EECP complements other therapies like skincare, diet, and exercise.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As an expert in treating patients with lifestyle disorders, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar serves as the Founder of FIT MY HEART and works as a Consultant at NEXIN HEALTH and MD CITY Hospital Noida. His extensive experience in cardiovascular care and innovative non-surgical treatment approaches makes him a leading authority in integrated EECP therapy applications combined with holistic healing methods.
His practice focuses on providing comprehensive alternatives to traditional cardiac interventions, helping patients achieve optimal cardiovascular health through evidence-based non-surgical treatments combined with lifestyle optimization and natural healing approaches.
For more information about integrated non-surgical cardiac treatments and comprehensive cardiovascular health services, visit www.viveksengar.in.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurvedic Heart Blockage Treatment
Revolutionary Non-Surgical Heart Treatment
References:
- World Health Organization – Global Health and Aging Report 2024
- International EECP Patient Registry – Anti-Aging Applications
- Journal of Anti-Aging Medicine – EECP Longevity Studies
- American College of Cardiology – Enhanced External Counterpulsation Guidelines
- European Society of Anti-Aging Medicine – Non-invasive Therapies
- Circulation Research – Cardiovascular Aging Mechanisms
- Nature Aging – Therapeutic Interventions for Healthy Longevity
- Clinical Interventions in Aging – EECP Applications in Geriatrics