EECP Therapy for Ischemic Cardiomyopathy: Ischemic cardiomyopathy represents one of the most challenging cardiac conditions affecting millions worldwide. When traditional treatments reach their limits, Enhanced External Counterpulsation (EECP) emerges as a beacon of hope. This groundbreaking non-invasive therapy is transforming how we approach heart muscle damage caused by inadequate blood supply.Heart disease continues to dominate global mortality statistics, with coronary artery disease being the primary culprit behind heart failure cases. For patients with ischemic cardiomyopathy, finding effective treatment options becomes crucial for maintaining quality of life and preventing disease progression.
Global Statistics: The Growing Burden of Ischemic Cardiomyopathy
The global prevalence of ischemic heart disease is rising, with current prevalence rates of 1,655 per 100,000 population expected to exceed 1,845 by 2030. These alarming statistics highlight the urgent need for innovative treatment approaches.
Ischemic heart disease affects approximately 7.6% of adult men globally, compared to 5.0% of adult women, making it the leading cause of death for both genders worldwide. The condition’s prevalence varies significantly across regions, with Eastern European countries sustaining the highest rates.
Long-term Impact Analysis
The long-term implications of ischemic cardiomyopathy extend far beyond individual health concerns. Healthcare systems globally face mounting pressure as the disease burden increases. Economic costs associated with heart failure management, including hospitalizations, medications, and lost productivity, create substantial financial strain on both families and healthcare infrastructure.
Progressive heart muscle damage leads to decreased cardiac output, exercise intolerance, and reduced life expectancy. Without effective intervention, patients experience declining functional capacity, frequent hospitalizations, and deteriorating quality of life. The condition’s progressive nature demands early intervention to prevent irreversible cardiac damage.
Understanding Ischemic Cardiomyopathy: Clinical Pathways and Pathogenesis
Disease Progression Mechanisms
Ischemic cardiomyopathy develops through a complex cascade of events initiated by inadequate coronary blood flow. The pathogenesis begins with atherosclerotic plaque formation in coronary arteries, leading to progressive vessel narrowing. This restriction reduces oxygen and nutrient delivery to myocardial tissue.
Chronic ischemia triggers several destructive processes within heart muscle cells. Oxidative stress increases, cellular energy production decreases, and inflammatory responses activate. These mechanisms collectively contribute to myocyte dysfunction, apoptosis, and eventual replacement with fibrous tissue.
Pathophysiological Changes
The heart undergoes significant structural and functional adaptations during ischemic cardiomyopathy progression. Initially, compensatory mechanisms attempt to maintain cardiac output through increased heart rate and ventricular wall thickening. However, these adaptations eventually become maladaptive.
Ventricular remodeling occurs as damaged areas develop into akinetic or dyskinetic segments. The remaining viable myocardium works harder to compensate, leading to further energy demands and potential ischemia. This vicious cycle perpetuates disease progression and functional deterioration.
Neurohormonal activation plays a crucial role in disease advancement. The renin-angiotensin-aldosterone system and sympathetic nervous system become hyperactive, causing vasoconstriction, fluid retention, and increased cardiac workload. These changes further compromise cardiac function and accelerate heart failure development.
EECP Treatment for Ischemic Cardiomyopathy: Revolutionary Therapeutic Approach
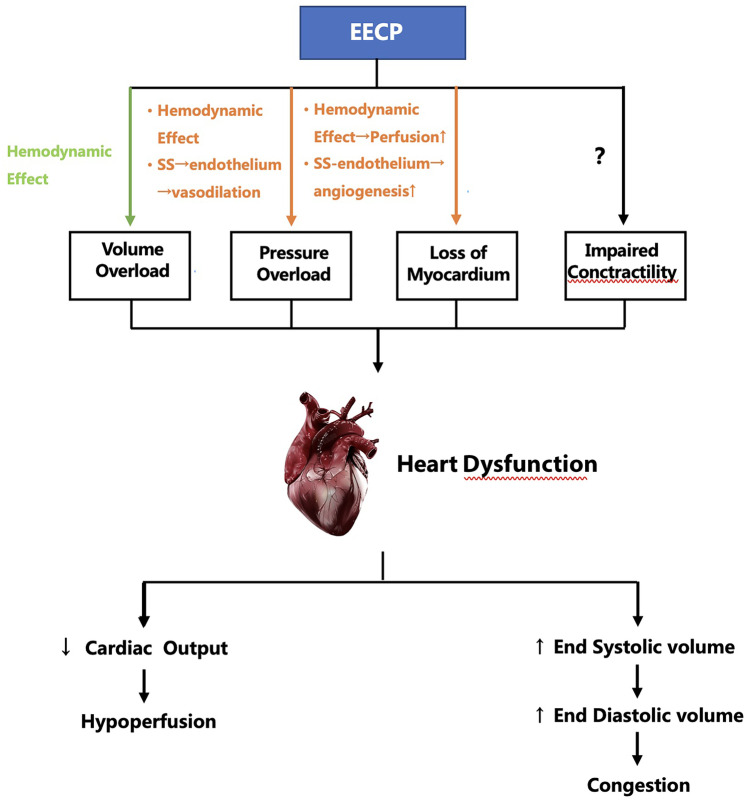
Enhanced External Counterpulsation represents a paradigm shift in treating ischemic cardiomyopathy without surgical intervention. This innovative therapy utilizes pneumatic cuffs placed around the patient’s legs and lower torso to enhance cardiac perfusion through synchronized inflation and deflation.
Mechanism of Action
EECP therapy works by increasing coronary blood flow during diastole while reducing cardiac workload during systole. The sequential compression of lower extremity vessels creates retrograde arterial flow, augmenting diastolic pressure and coronary perfusion. This mechanism promotes collateral circulation development and improves myocardial oxygen supply.
The therapy stimulates endothelial function improvement through increased shear stress on arterial walls. Enhanced nitric oxide production leads to improved vasodilation and reduced vascular resistance. These changes contribute to better blood flow distribution and cardiac performance optimization.
EECP vs. Alternative Treatments: Comprehensive Comparison
| Treatment Approach | Invasiveness | Success Rate | Duration | Side Effects | Recovery Time |
|---|---|---|---|---|---|
| EECP Therapy | Non-invasive | 85% improvement | 7 weeks | Minimal | Immediate |
| Coronary Bypass | Highly invasive | 90-95% | Single procedure | Significant | 6-12 weeks |
| Angioplasty | Minimally invasive | 70-80% | Single procedure | Moderate | 1-2 weeks |
| Medical Therapy | Non-invasive | 60-70% | Lifelong | Variable | N/A |
| Heart Transplant | Highly invasive | 85-90% | Single procedure | High | 6+ months |
Benefits of EECP Over Conventional Approaches
EECP therapy offers unique advantages compared to traditional ischemic cardiomyopathy treatments. The non-invasive nature eliminates surgical risks, making it suitable for high-risk patients who cannot undergo invasive procedures. Unlike bypass surgery or angioplasty, EECP carries no risk of procedural complications or anesthesia-related adverse events.
Clinical trials demonstrate that 85% of patients involved in EECP treatment experienced significant reduction in angina episodes and improved exercise tolerance. This success rate rivals many invasive procedures while maintaining excellent safety profiles.
The therapy’s accessibility makes it an attractive option for patients with multiple comorbidities or those deemed unsuitable for surgical intervention. Treatment can be administered on an outpatient basis, allowing patients to maintain normal daily activities throughout the treatment course.
Who Needs EECP Treatment for Ischemic Cardiomyopathy?
Primary Candidates
Patients with symptomatic ischemic cardiomyopathy who experience persistent angina despite optimal medical therapy represent ideal EECP candidates. This includes individuals with chronic stable angina, exercise intolerance, and reduced functional capacity due to coronary artery disease.
Elderly patients with multiple cardiovascular risk factors often benefit significantly from EECP therapy. Advanced age, diabetes, kidney disease, or previous cardiac procedures may preclude invasive treatments, making EECP an excellent alternative option.
Secondary Indications
Post-bypass surgery patients experiencing recurrent symptoms may find relief through EECP therapy. The treatment can address new blockages or incomplete revascularization without requiring additional surgical procedures. Similarly, patients with unsuccessful angioplasty results or restenosis can benefit from enhanced collateral circulation development.
Individuals with heart failure symptoms related to ischemic cardiomyopathy often experience improved quality of life following EECP treatment. The therapy’s ability to enhance cardiac output and reduce symptoms makes it valuable for managing chronic heart failure.
EECP Treatment Protocol and Methodology
Standard Treatment Course
The typical EECP treatment protocol involves 35 sessions administered over seven weeks. Each session lasts approximately one to two hours, with treatments scheduled five days per week. This standardized approach ensures optimal therapeutic benefits while maintaining patient comfort and safety.
During treatment, patients lie comfortably on a treatment bed with pneumatic cuffs wrapped around their legs and lower torso. The EECP device synchronizes cuff inflation with the patient’s cardiac cycle, monitored through continuous electrocardiogram recording.
Monitoring and Safety Measures
Comprehensive patient monitoring throughout EECP therapy ensures treatment safety and effectiveness. Blood pressure, heart rate, and oxygen saturation are continuously monitored during each session. Trained technicians adjust treatment parameters based on individual patient responses and tolerance levels.
Safety protocols include screening for contraindications such as severe aortic insufficiency, uncontrolled hypertension, or active blood clots. Patients undergo thorough cardiovascular assessment before initiating therapy to ensure appropriate candidate selection.
Clinical Evidence and Research Findings
Systematic Review Results
Recent systematic reviews demonstrate that standard EECP courses are safe in patients with ischemic heart failure and can significantly improve quality of life. These findings provide strong evidence supporting EECP’s therapeutic value in ischemic cardiomyopathy management.
Multiple clinical trials have evaluated EECP effectiveness in various patient populations. Studies consistently show improvements in angina frequency, exercise tolerance, and functional capacity following treatment completion. The therapy’s benefits often persist for extended periods after treatment conclusion.
Mechanisms of Improvement
Research reveals multiple pathways through which EECP therapy benefits ischemic cardiomyopathy patients. Enhanced coronary collateral circulation development represents the primary mechanism, providing alternative blood supply routes to ischemic myocardium. This collateral development often continues progressing even after treatment completion.
Improved endothelial function contributes significantly to treatment benefits. EECP-induced shear stress stimulates nitric oxide production, enhancing vasodilation and reducing vascular resistance. These changes improve overall cardiovascular function and reduce cardiac workload.
Physiological Effects of EECP on Cardiac Function
Hemodynamic Improvements
EECP therapy produces immediate and long-term hemodynamic benefits in ischemic cardiomyopathy patients. Acute effects include increased diastolic pressure augmentation, improved coronary perfusion, and reduced left ventricular workload. These changes optimize myocardial oxygen supply-demand balance.
Long-term hemodynamic improvements result from enhanced collateral circulation and improved endothelial function. Patients often demonstrate increased exercise capacity, reduced resting heart rate, and improved blood pressure control following treatment completion.
Myocardial Perfusion Enhancement
Advanced imaging studies reveal significant improvements in myocardial perfusion following EECP therapy. Nuclear perfusion scans demonstrate increased blood flow to previously ischemic regions, indicating successful collateral development. These perfusion improvements correlate with symptom reduction and functional capacity enhancement.
Regional wall motion abnormalities may show improvement in some patients following EECP treatment. Enhanced perfusion can restore contractile function in hibernating myocardium, leading to improved overall cardiac performance.
Contraindications and Patient Selection Criteria
Absolute Contraindications
Certain conditions preclude EECP therapy due to safety concerns. Severe aortic insufficiency represents an absolute contraindication, as diastolic augmentation could worsen regurgitation. Uncontrolled severe hypertension requires blood pressure optimization before considering EECP treatment.
Active venous thromboembolism or severe peripheral arterial disease affecting lower extremities may contraindicate therapy. Patients with severe heart failure requiring inotropic support typically require stabilization before EECP consideration.
Relative Contraindications
Moderate aortic stenosis requires careful evaluation before initiating EECP therapy. The treatment’s hemodynamic effects may not be appropriate for patients with significant outflow tract obstruction. Similarly, severe mitral regurgitation needs assessment to determine therapy suitability.
Pregnancy represents a relative contraindication due to limited safety data in expectant mothers. Patients with implanted cardiac devices require individual evaluation to ensure device compatibility with EECP equipment.
Integration with Comprehensive Cardiac Care
Multidisciplinary Approach
Optimal ischemic cardiomyopathy management requires coordinated multidisciplinary care. EECP therapy integrates seamlessly with existing cardiac rehabilitation programs, medication management, and lifestyle modification initiatives. This comprehensive approach maximizes therapeutic benefits and improves long-term outcomes.
Collaboration between cardiologists, EECP specialists, and cardiac rehabilitation teams ensures continuity of care. Regular communication among healthcare providers facilitates treatment optimization and monitoring of patient progress throughout the therapeutic process.
Lifestyle Modifications
EECP therapy effectiveness increases when combined with appropriate lifestyle modifications. Dietary counseling focusing on heart-healthy nutrition principles supports overall cardiovascular health improvement. Regular physical activity, within individual capacity limits, enhances treatment benefits and promotes long-term wellness.
Smoking cessation represents a crucial component of comprehensive ischemic cardiomyopathy management. Tobacco use cessation programs should be integrated with EECP therapy to maximize therapeutic benefits and prevent disease progression.
Future Directions and Research Opportunities
Emerging Applications
Research continues exploring expanded EECP applications in cardiovascular medicine. Studies investigate therapy effectiveness in different patient populations, including those with diabetes, kidney disease, and peripheral arterial disease. These investigations may broaden treatment indications and benefit more patients.
Combination therapies incorporating EECP with other non-invasive treatments show promising potential. Research exploring EECP combined with exercise training, nutritional interventions, or novel medications may enhance therapeutic outcomes.
Technological Advances
EECP technology continues evolving with improved monitoring capabilities and treatment customization options. Advanced hemodynamic monitoring systems provide real-time feedback for treatment optimization. These technological improvements enhance treatment effectiveness and patient safety.
Portable EECP devices under development may increase treatment accessibility and convenience. Home-based therapy options could expand treatment availability while reducing healthcare costs and improving patient compliance.
Quality of Life Improvements
Functional Capacity Enhancement
Patients undergoing EECP therapy frequently report significant improvements in daily functional capacity. Activities previously limited by angina or dyspnea become more manageable following treatment completion. These improvements translate into enhanced independence and better quality of life.
Exercise tolerance improvements allow patients to participate in activities they previously avoided. Walking distances increase, stair climbing becomes easier, and recreational activities become possible again. These changes contribute to improved psychological well-being and social engagement.
Symptom Relief
Angina reduction represents one of the most significant benefits reported by EECP patients. Chest pain frequency and intensity typically decrease substantially following treatment completion. This symptom relief reduces anxiety and fear associated with cardiac symptoms.
Dyspnea improvements allow better participation in daily activities and exercise. Patients often report increased energy levels and reduced fatigue, contributing to overall quality of life enhancement. Sleep quality may also improve as cardiac symptoms diminish.
Long-term Outcomes and Prognosis
Durability of Benefits
EECP therapy benefits often persist for extended periods following treatment completion. Studies demonstrate sustained improvements in angina frequency, exercise tolerance, and quality of life measures for months to years after therapy conclusion. This durability makes EECP a valuable long-term therapeutic option.
Collateral circulation development continues progressing even after active treatment ends. This ongoing improvement may provide additional benefits over time, potentially delaying or preventing the need for more invasive interventions.
Repeat Treatment Considerations
Some patients may benefit from repeat EECP courses if symptoms recur over time. The therapy’s excellent safety profile allows for multiple treatment courses when clinically indicated. Repeat treatments often provide similar benefits to initial therapy courses.
Factors influencing the need for repeat treatment include disease progression severity, adherence to lifestyle modifications, and optimal medical therapy compliance. Regular follow-up assessments help determine appropriate timing for potential repeat treatments.
Conclusion
EECP therapy represents a revolutionary advancement in ischemic cardiomyopathy treatment, offering hope to patients who have exhausted traditional therapeutic options. The evidence demonstrates that EECP is safe and can significantly improve quality of life in patients with ischemic heart failure, making it an invaluable addition to modern cardiac care.
The non-invasive nature of EECP therapy, combined with its excellent safety profile and proven effectiveness, makes it an attractive treatment option for diverse patient populations. As research continues expanding our understanding of optimal patient selection and treatment protocols, EECP therapy will likely play an increasingly important role in comprehensive ischemic cardiomyopathy management.
For patients struggling with persistent cardiac symptoms despite optimal medical therapy, EECP offers a path toward improved quality of life and enhanced functional capacity. The therapy’s ability to stimulate natural healing processes through collateral circulation development provides lasting benefits that extend well beyond the treatment period.
Healthcare providers managing ischemic cardiomyopathy patients should consider EECP therapy as part of comprehensive treatment planning. The therapy’s integration with existing cardiac care programs creates synergistic effects that maximize therapeutic benefits and improve long-term patient outcomes.
About the Author
Mr. Vivek Singh Sengar is a renowned clinical nutritionist and researcher with extensive expertise in EECP therapy and clinical nutrition. As the founder of FIT MY HEART and consultant at NEXIN HEALTH and MD CITY Hospital Noida, he has successfully treated over 25,000 patients suffering from heart disease and diabetes across the globe.
Mr. Sengar specializes in treating patients with lifestyle disorders and has dedicated his career to advancing non-invasive cardiac treatments. His comprehensive approach combines cutting-edge EECP therapy with personalized nutritional interventions to optimize patient outcomes.
For expert consultation on EECP therapy and comprehensive cardiac care, visit www.viveksengar.in to learn more about innovative treatment options for ischemic cardiomyopathy and other cardiovascular conditions.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurverdic Heart Blockage Treatment
Revolutionary Non Surgical Heart Treatment
Frequently Asked Questions: EECP Therapy for Ischemic Cardiomyopathy
Que: What is EECP therapy and how does it help patients with ischemic cardiomyopathy?
Ans: EECP Therapy is a clinically proven, non-invasive treatment for angina, chest pain, coronary artery disease, and heart failure. For ischemic cardiomyopathy patients, EECP improves coronary blood flow, reduces cardiac workload, and promotes collateral circulation development to help damaged heart muscle recover function.
Que: How effective is EECP therapy in improving symptoms of ischemic cardiomyopathy?
Ans: After completion of treatment, there was a significant decrease in severity of angina class (p < 0.001), and 72% improved from severe angina to no angina or mild angina. Studies show EECP significantly improves quality of life, exercise tolerance, and reduces hospitalization rates in ischemic cardiomyopathy patients.
Que: Can EECP therapy improve ejection fraction in patients with ischemic cardiomyopathy?
Ans: The effect of EECP on systolic function is still unclear, while EECP has a significant improvement effect on cardiac diastolic function While ejection fraction improvements vary, EECP consistently enhances diastolic function, reduces symptoms, and improves overall cardiac performance in ischemic cardiomyopathy patients.
Que: Is EECP therapy safe for patients with reduced ejection fraction due to ischemic cardiomyopathy?
Ans: Data from the International EECP Patient Registry show that patients with reduced left ventricular function (< 35%) achieved similar reductions in angina as those with preserved ejection fraction. EECP is safe and effective even in patients with severely reduced ejection fraction when properly monitored.
Que: How long does a complete EECP treatment course take for ischemic cardiomyopathy patients?
Ans: The standard EECP protocol consists of 35 – 40 one-hour sessions administered over 7 weeks, typically 5 days per week. Ischemic cardiomyopathy patients follow the same protocol, though some may require modified schedules based on their individual condition and response to treatment.
Que: What makes ischemic cardiomyopathy patients good candidates for EECP therapy?
Ans: Ideal candidates include patients with persistent heart failure symptoms despite optimal medical therapy, those not suitable for revascularization procedures, and patients with diffuse coronary disease. EECP is particularly beneficial for elderly patients or those with multiple comorbidities who cannot undergo surgery.
Que: Can EECP therapy be combined with standard heart failure medications for ischemic cardiomyopathy?
Ans: Yes, EECP safely complements standard heart failure medications including ACE inhibitors, beta-blockers, diuretics, and newer therapies like SGLT2 inhibitors. The combination often provides enhanced symptom relief and improved outcomes compared to medication alone.
Que: How does EECP therapy work to improve blood flow in ischemic cardiomyopathy?
Ans: EECP uses pneumatic cuffs around the legs that inflate during heart relaxation, forcing blood back to the coronary arteries. This enhanced coronary perfusion delivers more oxygen to damaged heart muscle while simultaneously reducing the heart’s workload during contraction.
Que: What symptoms of ischemic cardiomyopathy can improve with EECP therapy?
Ans: This treatment can reduce the re-hospitalization rate and emergency visit rate of patients within 6 months EECP commonly improves shortness of breath, chest pain, fatigue, exercise intolerance, and overall quality of life in ischemic cardiomyopathy patients.
Que: Are there any contraindications for EECP in ischemic cardiomyopathy patients?
Ans: Absolute contraindications include severe aortic insufficiency, uncompensated heart failure with fluid overload, and significant peripheral arterial disease. Patients with recent heart attacks, uncontrolled arrhythmias, or active infections should not receive EECP therapy.
Que: How soon can ischemic cardiomyopathy patients expect to see results from EECP therapy?
Ans: Many patients notice initial improvement in symptoms within 2-3 weeks of starting treatment. However, maximum benefits typically occur after completing the full 35-session course, with continued improvement for several weeks following treatment completion.
Que: Can EECP therapy help ischemic cardiomyopathy patients who have already had bypass surgery?
Ans: As a non-invasive treatment modality EECP is very effective in improving the symptoms of angina and heart failure when combined with medical treatment in patients with ICM after CABG. EECP is particularly beneficial for post-surgical patients with graft failure or progression of native vessel disease.
Que: What monitoring is required during EECP treatment for ischemic cardiomyopathy patients?
Ans: Continuous cardiac monitoring includes ECG surveillance, blood pressure measurement, and oxygen saturation monitoring. Heart failure patients require careful assessment of fluid status, daily weights, and symptoms to prevent treatment-related complications.
Que: How long do the benefits of EECP therapy last in ischemic cardiomyopathy patients?
Ans: Clinical studies demonstrate that EECP benefits typically persist for 2-5 years following treatment completion. Some patients may require repeat courses to maintain optimal benefits, especially those with progressive coronary disease or advancing heart failure.
Que: Can EECP therapy reduce the need for heart transplantation in ischemic cardiomyopathy patients?
Ans: While EECP cannot replace the need for heart transplantation in end-stage disease, it may help stabilize patients, improve their quality of life, and potentially serve as a bridge therapy while awaiting transplantation. Some patients may experience sufficient improvement to delay or avoid transplantation consideration.
References
- Zhang, Y., et al. (2023). The Effect of EECP on Ischemic Heart Failure: a Systematic Review. Current Cardiology Reports.
- Global Burden of Disease Study. (2024). Global, Regional, and National Time Trends in Ischemic Heart Disease Mortality. JMIR Public Health and Surveillance.
- American Heart Association. (2024). Heart Disease and Stroke Statistics: A Report of US and Global Data. Circulation.
- Manchanda, A., et al. (2018). Enhanced external counterpulsation in ischemic cardiomyopathy after coronary artery bypass grafting. International Journal of Cardiology.
- Bondesson, S., et al. (2008). Enhanced external counterpulsation in ischemic heart disease and congestive heart failure. Canadian Medical Association Journal.
- Wu, G., et al. (2007). Effects of long-term EECP treatment on exercise capacity in patients with coronary artery disease. American Journal of Cardiology.
- Lawson, W., et al. (1996). Efficacy of enhanced external counterpulsation in the treatment of angina pectoris. American Journal of Cardiology.
- European Society of Cardiology. (2023). Guidelines for the management of cardiomyopathies. European Heart Journal.