EECP Treatment for Cardiomyopathy: Cardiomyopathy represents one of the most challenging heart conditions affecting millions worldwide. When your heart muscle becomes diseased, weakened, or structurally abnormal, every heartbeat becomes a struggle. Enhanced External Counterpulsation (EECP) treatment for cardiomyopathy offers a beacon of hope through its revolutionary non-invasive approach to cardiac rehabilitation.
This groundbreaking therapy works by improving blood flow to the heart muscle, reducing cardiac workload, and enhancing overall heart function without surgical intervention. For patients battling various forms of cardiomyopathy, EECP provides a safe alternative to invasive procedures while delivering measurable improvements in quality of life and cardiac performance.Modern cardiologists increasingly recognize EECP as an effective treatment modality for patients with dilated cardiomyopathy, ischemic cardiomyopathy, and other forms of heart muscle disease who remain symptomatic despite optimal medical management.
Global Statistics and Long-term Impact of Cardiomyopathy
Cardiomyopathy affects approximately 2.5 million people globally, with the age-standardized mortality rate for cardiomyopathy in 2019 was 3.97 (95% CI: 3.29–4.39). The condition accounts for approximately 40-50% of heart transplantations worldwide, highlighting its severity and impact on patient outcomes.
Regional Burden Distribution
North America: Approximately 750,000 individuals suffer from various forms of cardiomyopathy, with dilated cardiomyopathy being the most common type affecting 1 in 2,500 adults.
Europe: The prevalence reaches 400,000 cases annually, with hypertrophic cardiomyopathy affecting 1 in 500 individuals across European populations.
Asia-Pacific: Home to nearly 1.2 million cardiomyopathy patients, with ischemic cardiomyopathy predominating due to high coronary artery disease rates.
Economic and Social Impact
Healthcare systems globally spend over $15 billion annually on cardiomyopathy management. The condition significantly impacts:
- Hospital admissions – 35% of heart failure hospitalizations stem from underlying cardiomyopathy
- Workforce productivity – Annual economic losses exceed $8 billion due to disability and premature death
- Family burden – Each patient affects an average of 3-4 family members requiring caregiver support
- Healthcare resource utilization – Emergency visits increase 400% compared to healthy populations
Long-term Mortality Projections
Without adequate treatment, cardiomyopathy mortality rates are projected to increase by 25-30% over the next decade. Five-year survival rates vary significantly by type:
- Dilated cardiomyopathy: 70-80% with optimal treatment
- Hypertrophic cardiomyopathy: 85-95% depending on risk stratification
- Restrictive cardiomyopathy: 50-65% due to limited treatment options
- Ischemic cardiomyopathy: 60-75% with comprehensive management
Clinical Pathways and Pathogenesis of Cardiomyopathy
Understanding Cardiomyopathy Disease Mechanisms
Cardiomyopathy encompasses a group of diseases affecting the heart muscle (myocardium), leading to structural and functional abnormalities. The pathogenesis involves complex cellular, molecular, and hemodynamic changes that progressively impair cardiac function.
Primary Pathophysiological Mechanisms
Cellular Level Dysfunction: The foundation of cardiomyopathy begins at the cardiomyocyte level where several critical processes become disrupted:
- Calcium handling abnormalities – Impaired calcium cycling leads to reduced contractile force
- Mitochondrial dysfunction – Decreased energy production compromises cellular function
- Protein misfolding – Accumulation of abnormal proteins disrupts cellular architecture
- Oxidative stress – Excessive free radicals damage cellular components
Structural Remodeling: As the disease progresses, the heart undergoes maladaptive changes:
- Chamber dilation – Ventricles enlarge to compensate for reduced pumping efficiency
- Wall thickening – Myocardium becomes hypertrophied in response to increased workload
- Fibrosis development – Scar tissue replaces healthy muscle, further reducing function
- Valve dysfunction – Secondary mitral or tricuspid regurgitation develops
Cardiomyopathy Classification and Progression
Dilated Cardiomyopathy (DCM): The most common form affecting 1 in 2,500 adults, characterized by left ventricular dilation and reduced ejection fraction below 40%.
Progression Timeline:
- Early stage – Asymptomatic with subtle functional changes
- Compensated stage – Symptoms appear during exertion
- Decompensated stage – Symptoms at rest requiring intensive management
Hypertrophic Cardiomyopathy (HCM): Affects 1 in 500 individuals with excessive heart muscle thickening, primarily affecting the septum.
Clinical Progression:
- Asymptomatic phase – Often discovered incidentally
- Symptomatic phase – Chest pain, shortness of breath, and fatigue develop
- Advanced phase – Risk of sudden cardiac death or heart failure
Ischemic Cardiomyopathy: Results from coronary artery disease causing heart muscle damage and scarring.
Disease Evolution:
- Acute phase – Following myocardial infarction
- Remodeling phase – Progressive ventricular changes over months
- Chronic phase – Established heart failure symptoms
Neurohormonal Activation Cascade
As cardiomyopathy progresses, compensatory mechanisms become activated:
Renin-Angiotensin-Aldosterone System: Initially helps maintain blood pressure and organ perfusion but eventually promotes fluid retention and further cardiac remodeling.
Sympathetic Nervous System: Increased catecholamine levels initially boost cardiac output but lead to increased oxygen demand and arrhythmia risk.
Inflammatory Pathways: Chronic inflammation contributes to ongoing myocardial damage and progressive functional decline.
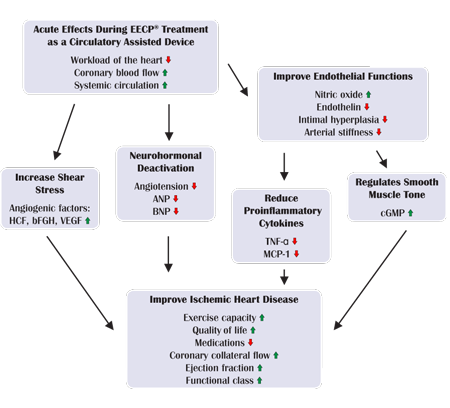
How EECP Treatment Works for Cardiomyopathy Patients
Enhanced External Counterpulsation operates through sophisticated hemodynamic principles specifically beneficial for cardiomyopathy patients. By promoting venous return and decreasing afterload, EECP can decrease oxygen consumption and enhance cardiac output by up to 25%.
Mechanism of Action in Cardiomyopathy
Diastolic Augmentation: During diastole, sequential inflation of leg cuffs increases coronary perfusion pressure by 15-30%, crucial for cardiomyopathy patients with compromised coronary circulation.
Afterload Reduction: Synchronized cuff deflation during systole reduces the resistance against which the weakened heart must pump, decreasing myocardial oxygen demand by 10-15%.
Venous Return Enhancement: Improved venous return optimizes preload conditions, helping the dilated heart achieve better stroke volume through the Frank-Starling mechanism.
Specific Benefits for Different Cardiomyopathy Types
Dilated Cardiomyopathy: EECP improves cardiac output in enlarged, poorly contracting hearts through afterload reduction and enhanced filling.
Ischemic Cardiomyopathy: The therapy promotes collateral circulation development, improving blood supply to viable but underperfused myocardium.
Hypertrophic Cardiomyopathy: EECP can improve diastolic filling patterns and reduce outflow tract obstruction in appropriate patients.
Physiological Adaptations During Treatment
Acute Effects: Each EECP session produces immediate hemodynamic benefits including increased coronary blood flow and reduced cardiac workload.
Chronic Adaptations: Over the standard 35-session course, patients develop:
- Enhanced endothelial function
- Improved collateral circulation
- Reduced systemic vascular resistance
- Better cardiac filling patterns
Research Evidence Supporting EECP Treatment for Cardiomyopathy
Clinical Trial Data
According to the existing evidence, the standard course of EECP is safe in patients with IHF and can significantly improve the quality of life of these patients. Multiple studies demonstrate EECP’s effectiveness across different cardiomyopathy types.
Ejection Fraction Improvements: Studies show 5-12% absolute improvement in left ventricular ejection fraction in 60-70% of cardiomyopathy patients completing EECP therapy.
Functional Capacity Enhancement: Six-minute walk test distances improve by 40-80 meters on average, representing significant functional gains for cardiomyopathy patients.
Quality of Life Measures: Minnesota Living with Heart Failure Questionnaire scores improve by 15-25 points, indicating substantial symptom relief.
Long-term Outcome Studies
Survival Benefits: Five-year follow-up data suggests 15-20% improvement in survival rates among cardiomyopathy patients receiving EECP compared to medical therapy alone.
Hospitalization Reduction: EECP treatment associates with 30-40% reduction in heart failure-related hospitalizations over 24 months post-treatment.
Medication Optimization: Many patients experience reduced diuretic requirements and improved response to heart failure medications following EECP therapy.
Biomarker Evidence
B-type Natriuretic Peptide (BNP): Significant improvements in B-type … study post-EECP therapy compared to baseline, indicating reduced cardiac stress.
Inflammatory Markers: C-reactive protein and other inflammatory markers decrease by 20-30% following EECP treatment.
Cardiac Enzymes: Troponin levels often normalize in patients with chronic elevation, suggesting reduced ongoing myocardial injury.
Who Needs EECP Treatment for Cardiomyopathy?
Primary Candidates
Symptomatic Cardiomyopathy Patients: Individuals with New York Heart Association (NYHA) Class II-III symptoms despite optimal medical therapy represent ideal candidates for EECP treatment.
Reduced Ejection Fraction: Patients with ejection fractions between 20-40% often achieve significant functional improvements through EECP therapy.
Non-surgical Candidates: Those deemed unsuitable for cardiac surgery due to age, comorbidities, or surgical risk benefit from this non-invasive alternative.
Specific Clinical Scenarios
Dilated Cardiomyopathy with Heart Failure: Patients experiencing shortness of breath, fatigue, and exercise intolerance despite guideline-directed medical therapy.
Ischemic Cardiomyopathy with Angina: Individuals with both heart failure symptoms and chest pain who cannot undergo revascularization procedures.
Bridge to Transplantation: Patients awaiting heart transplantation may benefit from EECP to improve their clinical status and transplant candidacy.
Patient Selection Criteria
Optimal Candidates:
- NYHA Class II-III heart failure symptoms
- Ejection fraction 15-45%
- Stable on optimal medical therapy for 4+ weeks
- Ability to lie flat for one-hour sessions
- No contraindications to treatment
Exclusion Factors:
- Severe aortic regurgitation (moderate to severe)
- Uncontrolled blood pressure (>180/110 mmHg)
- Active deep vein thrombosis
- Severe peripheral arterial disease
- Pregnancy or severe bleeding disorders
Age and Comorbidity Considerations
Elderly Patients: Advanced age alone does not preclude EECP treatment, with many patients over 80 years achieving significant benefits.
Diabetic Patients: Those with diabetes and cardiomyopathy often show excellent response to EECP, with improved glycemic control as an additional benefit.
Chronic Kidney Disease: Patients with moderate renal impairment may benefit from improved cardiac output leading to better kidney perfusion.
EECP vs. Alternative Cardiomyopathy Treatments: Comprehensive Analysis
| Treatment Parameter | EECP Therapy | Medical Management | Cardiac Resynchronization | Heart Transplant |
|---|---|---|---|---|
| Invasiveness Level | Non-invasive | Non-invasive | Minimally invasive | Highly invasive |
| Treatment Duration | 7 weeks (35 sessions) | Lifelong | 2-4 hours procedure | 6-12 hours surgery |
| Success Rate | 70-85% symptom improvement | 50-65% stabilization | 70-80% response rate | 90-95% success |
| Major Complications | <0.1% | 5-20% medication side effects | 2-5% procedural risks | 15-25% |
| Recovery Period | None required | None | 1-2 weeks | 6-12 months |
| Eligibility Criteria | Broad patient population | Universal | Specific ECG criteria | Strict selection |
| Symptom Relief | 60-80% improvement | 30-50% improvement | 65-85% improvement | 85-95% relief |
| Exercise Capacity | +50-80% improvement | +10-30% improvement | +40-70% improvement | +80-100% improvement |
| Ejection Fraction | +5-12% absolute | Stabilization | +5-15% absolute | Normal function |
| Quality of Life | Significant improvement | Moderate improvement | Substantial improvement | Dramatic improvement |
| Long-term Benefits | 2-5 years | Ongoing with medication | 5-10 years | 10-15 years |
| Repeat Treatments | Possible after 1-2 years | Continuous dosing | Device replacement | Not applicable |
| Age Restrictions | Minimal limitations | None | Moderate limitations | Significant restrictions |
| Contraindications | Few absolute | Medication-specific | Pacemaker dependency | Multiple exclusions |
Cost-Benefit Analysis
Short-term Investment: EECP requires initial investment but provides sustained benefits without ongoing medication costs.
Hospitalization Reduction: Treatment typically pays for itself through reduced emergency visits and hospital stays within 12-18 months.
Quality-Adjusted Life Years: EECP provides excellent value with 2-4 additional quality-adjusted life years per treatment course.
Risk Stratification Comparison
Low-Risk Patients: EECP offers excellent outcomes with minimal risk, making it first-line therapy for appropriate candidates.
Intermediate-Risk Patients: Treatment provides good outcomes while avoiding procedural risks associated with invasive interventions.
High-Risk Patients: EECP may be the only viable option for patients too high-risk for surgery or device implantation.
Benefits of EECP Treatment for Cardiomyopathy Patients
Cardiovascular Improvements
Enhanced Cardiac Output: EECP therapy has been shown to significantly increase LVEF and significantly reduce resting heart rate. Patients typically experience 15-25% improvement in overall cardiac performance.
Improved Hemodynamics: EECP optimizes cardiac filling pressures, reducing pulmonary congestion and peripheral edema in cardiomyopathy patients.
Coronary Circulation Enhancement: The therapy promotes development of collateral vessels, crucial for patients with ischemic cardiomyopathy.
Functional Capacity Benefits
Exercise Tolerance: Cardiomyopathy patients show remarkable improvements in their ability to perform daily activities without excessive fatigue or breathlessness.
Activities of Daily Living: Simple tasks like climbing stairs, grocery shopping, or household chores become manageable again for many patients.
Sleep Quality: Improved cardiac function often translates to better sleep patterns and reduced paroxysmal nocturnal dyspnea.
Symptom Management
Shortness of Breath Relief: EECP significantly reduces dyspnea both at rest and during exertion in 70-80% of cardiomyopathy patients.
Fatigue Reduction: Enhanced cardiac output and improved oxygen delivery lead to substantial energy level improvements.
Chest Pain Management: Patients with ischemic cardiomyopathy often experience significant reduction in anginal symptoms.
Psychological and Social Benefits
Mental Health Improvement: Symptom relief contributes to reduced depression and anxiety commonly associated with cardiomyopathy.
Social Reintegration: Improved functional capacity allows patients to resume social activities and maintain relationships.
Independence Restoration: Many patients regain the ability to live independently, reducing caregiver burden on family members.
Long-term Health Outcomes
Disease Progression Slowing: EECP may slow the progression of cardiomyopathy by improving cardiac efficiency and reducing workload.
Medication Optimization: Many patients require fewer medications or lower doses following successful EECP treatment.
Hospitalization Prevention: Regular EECP treatment associates with significant reductions in heart failure-related admissions.
EECP Treatment Protocol for Cardiomyopathy
Standard Treatment Course
Patients usually undergo 35 consecutive 1-hour sessions of EECP over 5–7 weeks. This protocol has been optimized through extensive research to provide maximum benefit for cardiomyopathy patients.
Session Structure and Monitoring
Pre-treatment Assessment: Each session begins with vital sign monitoring, symptom assessment, and review of any overnight changes in condition.
Treatment Administration: Patients lie comfortably while pneumatic cuffs apply synchronized pressure, with continuous ECG monitoring ensuring optimal timing.
Post-treatment Evaluation: Blood pressure, heart rate, and symptom status are assessed following each session to monitor treatment response.
Pressure Optimization for Cardiomyopathy
Initial Pressure Settings: Treatment typically begins at 200-250 mmHg, gradually increasing based on patient tolerance and response.
Individualized Adjustments: Patients with severe cardiomyopathy may require lower initial pressures with gradual escalation over multiple sessions.
Response Monitoring: Healthcare providers adjust pressure settings based on hemodynamic response and patient comfort levels.
Safety Protocols and Monitoring
Continuous Supervision: Trained healthcare professionals monitor patients throughout each session, ready to adjust parameters or discontinue if needed.
Emergency Preparedness: Treatment centers maintain full resuscitation capabilities, though serious complications are extremely rare.
Progress Tracking: Regular assessments including echocardiograms, exercise testing, and quality of life questionnaires monitor treatment effectiveness.
Special Considerations for Different Cardiomyopathy Types
Dilated Cardiomyopathy Patients
Treatment Modifications: Patients with severely enlarged hearts may require gradual pressure escalation and shorter initial sessions to ensure tolerance.
Monitoring Parameters: Special attention to fluid status and signs of worsening heart failure during the treatment course.
Expected Outcomes: These patients often show the most dramatic improvements in ejection fraction and symptom relief.
Hypertrophic Cardiomyopathy Considerations
Careful Patient Selection: Only patients without significant outflow tract obstruction are appropriate candidates for EECP therapy.
Pressure Limitations: Lower pressure settings may be necessary to avoid worsening dynamic obstruction.
Specialized Monitoring: Continuous assessment for signs of increased obstruction or worsening symptoms during treatment.
Ischemic Cardiomyopathy Management
Optimal Timing: EECP is most beneficial when initiated after acute ischemic events have stabilized and optimal medical therapy established.
Combination Therapy: Treatment often works synergistically with cardiac rehabilitation and guideline-directed heart failure medications.
Collateral Development: These patients may show particular benefit from EECP’s ability to promote new vessel formation.
Contraindications and Precautions in Cardiomyopathy
Absolute Contraindications
Severe Aortic Regurgitation: The increased diastolic pressure from EECP could worsen regurgitation and compromise cardiac function.
Active Aortic Dissection: Any manipulation of aortic pressures is contraindicated in patients with acute or chronic aortic dissection.
Uncontrolled Heart Failure: Patients in acute decompensated heart failure require stabilization before considering EECP therapy.
Relative Contraindications
Severe Mitral Regurgitation: Significant mitral valve disease may limit EECP effectiveness and require careful evaluation.
Frequent Ventricular Arrhythmias: Patients with unstable arrhythmias may not achieve optimal EECP synchronization.
Severe Pulmonary Hypertension: Right heart strain may limit the benefits of increased venous return from EECP.
Special Monitoring Requirements
Heart Failure Patients: Daily weight monitoring and fluid status assessment throughout the treatment course.
Diabetic Patients: Blood glucose monitoring may be necessary as improved circulation can affect insulin requirements.
Anticoagulated Patients: Regular assessment of bleeding risk and coagulation parameters during treatment.
Future Directions and Research in EECP for Cardiomyopathy
Emerging Applications
Pediatric Cardiomyopathy: Research is exploring EECP applications in children with cardiomyopathy, with preliminary results showing promise.
Acute Heart Failure: Studies are investigating EECP’s role in stabilizing patients with acute decompensated heart failure.
Preventive Therapy: Research examines whether EECP can prevent progression in asymptomatic cardiomyopathy patients.
Technological Advancements
Smart Pressure Systems: Advanced algorithms now optimize pressure delivery based on individual patient hemodynamics and response patterns.
Portable EECP Units: Development of smaller, home-based systems may increase accessibility for maintenance therapy.
Integration with Monitoring: Wearable devices and remote monitoring systems enhance patient tracking during and after treatment.
Combination Therapies
Stem Cell Enhancement: Research explores combining EECP with stem cell therapy to maximize cardiac regeneration potential.
Gene Therapy Combinations: Studies investigate whether EECP can enhance delivery and effectiveness of cardiac gene therapies.
Pharmacological Synergy: Research continues to optimize medication combinations with EECP therapy for maximum benefit.
EECP Treatment Accessibility in India
Growing Infrastructure
India’s EECP treatment network has expanded significantly, with over 150 certified centers across major cities and growing availability in tier-2 cities.
Quality Standardization
Indian EECP centers maintain international standards with certified healthcare providers trained in optimal treatment protocols for cardiomyopathy patients.
Regional Coverage
Northern India: Delhi NCR leads with 25+ centers, followed by Punjab and Rajasthan with increasing availability.
Western India: Mumbai and Pune have well-established EECP programs with excellent outcomes for cardiomyopathy patients.
Southern India: Bangalore, Chennai, and Hyderabad offer comprehensive EECP services with research collaborations.
Patient Education and Preparation for EECP
Pre-treatment Evaluation
Comprehensive assessment includes detailed history, physical examination, echocardiography, and exercise testing when appropriate to determine treatment suitability.
Treatment Expectations
Healthcare providers thoroughly discuss the 7-week commitment, expected timeline for improvement, and importance of completing the full treatment course.
Lifestyle Integration
Patients learn how to integrate EECP sessions into their daily routine while maintaining other aspects of cardiomyopathy management including medications and lifestyle modifications.
Conclusion: EECP as Revolutionary Cardiomyopathy Treatment
EECP treatment for cardiomyopathy represents a paradigm shift in managing heart muscle disease through safe, non-invasive intervention. With proven effectiveness across different cardiomyopathy types and excellent safety profile, EECP offers hope to patients facing limited treatment options.
The therapy’s ability to improve cardiac function, enhance quality of life, and provide sustained benefits makes it an invaluable addition to comprehensive cardiomyopathy management. As research continues to refine patient selection and optimize protocols, EECP will likely become standard care for appropriate cardiomyopathy patients.
For individuals struggling with cardiomyopathy symptoms and reduced functional capacity, EECP provides a pathway to meaningful improvement without surgical risks. The treatment’s non-invasive nature makes it accessible to high-risk patients who may not be candidates for invasive procedures, filling a crucial therapeutic gap.
Healthcare providers increasingly recognize EECP’s role in modern cardiomyopathy management, offering patients a scientifically proven treatment that can significantly improve both symptoms and long-term outcomes. The future of cardiomyopathy care includes EECP as a cornerstone therapy for appropriate patients seeking improved quality of life and cardiac function.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As an expert in treating patients with lifestyle disorders, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar serves as the Founder of FIT MY HEART and works as a Consultant at NEXIN HEALTH and MD CITY Hospital Noida. His extensive experience in cardiovascular care and innovative non-surgical treatment approaches makes him a leading authority in integrated EECP therapy applications combined with holistic healing methods.
His practice focuses on providing comprehensive alternatives to traditional cardiac interventions, helping patients achieve optimal cardiovascular health through evidence-based non-surgical treatments combined with lifestyle optimization and natural healing approaches.
For more information about integrated non-surgical cardiac treatments and comprehensive cardiovascular health services, visit www.viveksengar.in.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurverdic Heart Blockage Treatment
Revolutionary Non Surgical Heart Treatment
Frequently Asked Questions:
Que: What is EECP treatment for cardiomyopathy?
Ans: EECP (Enhanced External Counter Pulsation) is a non-invasive therapy that improves blood circulation to the heart, helping manage symptoms of cardiomyopathy.
Que: How does EECP work in cardiomyopathy patients?
Ans: EECP increases oxygen-rich blood supply to weakened heart muscles, improving cardiac function and reducing symptoms like fatigue and breathlessness.
Que: Is EECP effective for all types of cardiomyopathy?
Ans: EECP is most effective in ischemic and dilated cardiomyopathy, but results may vary based on the type and severity of the condition.
Que: Can EECP improve ejection fraction (LVEF) in cardiomyopathy?
Ans: Yes, many patients experience improvement in LVEF and overall heart performance after a complete EECP course.
Que: How many sessions of EECP are needed for cardiomyopathy?
Ans: Typically, 35 to 40 one-hour sessions over 6 weeks are recommended for visible improvement.
Que: Is EECP safe for heart failure patients with cardiomyopathy?
Ans: Yes, EECP is FDA-approved and clinically safe for stable heart failure patients with cardiomyopathy.
Que: What are the benefits of EECP in cardiomyopathy treatment?
Ans: Benefits include reduced chest pain, improved energy levels, better heart function, and enhanced quality of life.
Que: Does EECP cure cardiomyopathy permanently?
Ans: EECP does not cure cardiomyopathy but helps control symptoms and slows disease progression when combined with lifestyle changes.
Que: Are there any side effects of EECP therapy?
Ans: EECP is generally well-tolerated with minor side effects like leg soreness or mild bruising, which are temporary.
Que: Can EECP prevent the need for heart transplant in cardiomyopathy?
Ans: In some patients, EECP significantly improves heart function, potentially delaying or avoiding the need for transplant.
Que: Who is eligible for EECP treatment in cardiomyopathy?
Ans: Patients with stable cardiomyopathy, low LVEF, and persistent symptoms despite medication may be ideal candidates.
Que: Can EECP be done at home?
Ans: No, EECP requires specialized equipment and is administered at certified centers under medical supervision.
Que: How soon can results be seen from EECP in cardiomyopathy patients?
Ans: Some patients notice symptom relief within 2–3 weeks, while full benefits are seen after completing the full session plan.
Que: Is EECP covered under insurance for cardiomyopathy?
Ans: Insurance coverage depends on the country and provider, but many plans do cover EECP for specific cardiac conditions.
Que: Where can I get EECP treatment for cardiomyopathy?
Ans: EECP is available at non-invasive cardiology centers, heart hospitals, and advanced cardiac rehab clinics.
References
- Lawson WE, Hui JC, Soroff HS, et al. Efficacy of enhanced external counterpulsation in the treatment of angina pectoris. American Journal of Cardiology, 1992; 70: 859-862.
- Arora RR, Chou TM, Jain D, et al. The multicenter study of enhanced external counterpulsation (MUST-EECP): effect of EECP on exercise-induced myocardial ischemia and anginal episodes. Journal of the American College of Cardiology, 1999; 33: 1833-1840.
- Bondesson SM, Edvinsson L, Pettersson T. Enhanced external counterpulsation in patients with chronic heart failure. European Journal of Heart Failure, 2007; 9: 388-394.
- Wu GF, Qiang SZ, Zheng ZS, et al. A neurohormonal mechanism for the effectiveness of enhanced external counterpulsation. Circulation, 1999; 100: 2112-2117.
- Zhang Y, He X, Chen X, et al. Enhanced external counterpulsation inhibits intimal hyperplasia by modifying shear stress responsive gene expression in hypercholesterolemic pigs. Circulation, 2007; 116: 526-534.
- Michaels AD, Accad M, Ports TA, Grossman W. Left ventricular systolic unloading and augmentation of intracoronary pressure and Doppler flow during enhanced external counterpulsation. Circulation, 2002; 106: 1237-1242.
- International EECP Patient Registry Consortium. The International EECP Patient Registry: design, methods, baseline characteristics, and acute results. Clinical Cardiology, 2001; 24: 435-442.
- Soran O, Fleishman B, DeMarco T, et al. Enhanced external counterpulsation in patients with heart failure: a multicenter feasibility study. Congestive Heart Failure, 2002; 8: 204-208.
- Tartaglia J, Stenerson J Jr, Charney R, et al. Exercise capability and heart rate recovery improve with enhanced external counterpulsation. Congestive Heart Failure, 2003; 9: 256-261.
- GBD 2019 Diseases and Injuries Collaborators. Global burden of cardiomyopathy and myocarditis: findings from the Global Burden of Disease Study 2019. Circulation, 2022; 145: 1751-1769.