Non Surgical Heart Treatment: Cardiovascular disease continues to challenge millions worldwide, forcing patients into difficult decisions between invasive procedures and compromised quality of life. Enhanced External Counterpulsation (EECP) therapy emerges as a groundbreaking solution, offering hope where traditional treatments may fall short. This comprehensive exploration reveals how EECP therapy transforms the landscape of cardiac care, providing a viable non-surgical treatment option that rivals conventional interventions.
Global Statistics of Cardiovascular Disease: A Growing Crisis
The magnitude of cardiovascular disease worldwide presents alarming figures that demand immediate attention. Global death counts due to cardiovascular disease increased from 12.4 million in 1990 to 19.8 million in 2022, reflecting not just population growth but also the escalating burden of preventable risk factors.
Current data reveals disturbing trends:
- CAD causes 40% of heart-related deaths annually, and every 40 seconds, someone in the United States has a CAD-caused heart attack
- About 1 in 20 adults age 20 and older have CAD (about 5%)
- Projections indicate a 90.0% increase in cardiovascular prevalence, 73.4% increase in crude mortality, and 54.7% increase in crude DALYs between 2025 and 2050
Long-term Impact of Current Statistics
These statistics paint a concerning picture of our cardiovascular future. The projected increase means healthcare systems worldwide will face unprecedented pressure. Traditional surgical interventions, while effective, cannot accommodate the growing patient population requiring cardiac care. This gap creates an urgent need for alternative treatment modalities like EECP therapy.
Economic implications are equally staggering. The American healthcare system spends over $200 billion annually on hospital care and medications for heart disease management. Non-surgical alternatives like EECP therapy offer potential solutions to reduce this financial burden while maintaining therapeutic efficacy.
Understanding EECP Therapy: The Revolutionary Non-Surgical Approach
Enhanced External Counterpulsation represents a paradigm shift in cardiac treatment methodology. EECP treatment is an FDA-approved outpatient therapy that can improve blood flow to your heart, offering patients a completely non-invasive option for managing complex cardiac conditions.
How EECP Works: The Science Behind Success
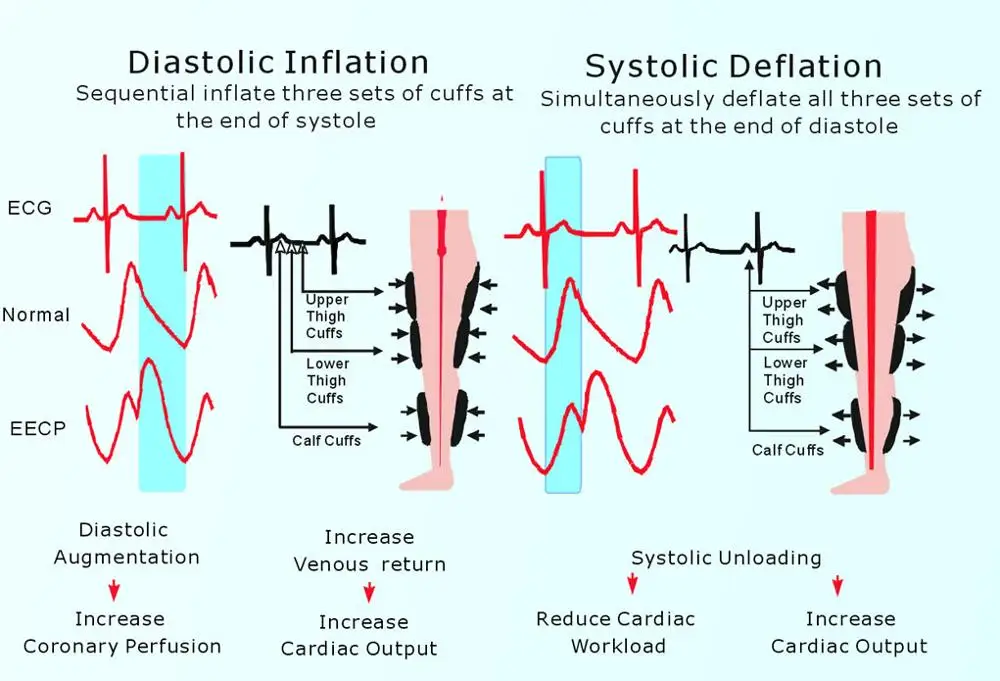
EECP therapy operates on sophisticated physiological principles that enhance natural cardiac function. During treatment, specialized pneumatic cuffs wrapped around the patient’s legs inflate and deflate in precise synchronization with the cardiac cycle. This coordinated compression creates a counterpulsation effect that dramatically improves coronary perfusion.
The mechanism involves three critical phases:
Diastolic Augmentation: During cardiac diastole, the cuffs inflate sequentially from calves to thighs, propelling blood toward the heart and increasing coronary artery filling pressure.
Systolic Unloading: As the heart contracts, cuffs rapidly deflate, reducing afterload and allowing the heart to pump more efficiently with less effort.
Collateral Development: Repeated sessions promote angiogenesis, encouraging the formation of natural bypass vessels around blocked arteries.
EECP Mechanism of Action – Vivek Sengar
Clinical Pathways and Pathogenesis
The pathogenesis of coronary artery disease involves complex inflammatory processes, endothelial dysfunction, and progressive atherosclerotic plaque formation. Traditional interventions like bypass surgery or stenting address the mechanical obstruction but may not address underlying pathophysiology.
EECP therapy works differently by:
- Enhancing endothelial function through increased shear stress
- Promoting nitric oxide production for vasodilation
- Stimulating angiogenic factors for natural collateral formation
- Reducing inflammatory markers associated with atherosclerosis
This comprehensive approach addresses both symptoms and underlying disease mechanisms, offering sustained therapeutic benefits.
Benefits of EECP Therapy: Evidence-Based Advantages
Research consistently demonstrates EECP therapy’s remarkable efficacy across multiple clinical parameters. Studies show that EECP improves blood flow and reduces symptoms of angina, with over 75% of patients experiencing a reduction in angina symptoms, providing substantial relief for patients with refractory chest pain.
Immediate Clinical Benefits
Patients typically experience significant improvements within the first few weeks of treatment:
Angina Reduction: The majority of patients report decreased frequency and intensity of chest pain episodes, often eliminating the need for rescue medications.
Exercise Tolerance: Enhanced cardiac output allows patients to engage in previously impossible physical activities, dramatically improving quality of life.
Medication Reduction: Many patients can reduce or eliminate cardiac medications under physician supervision, minimizing side effects and drug interactions.
Long-term Therapeutic Outcomes
Research has shown the beneficial effects of EECP Flow Therapy to last between two and five years after treatment, providing sustained relief that often exceeds the durability of some surgical interventions.
Long-term benefits include:
- Sustained improvement in cardiac function
- Reduced hospitalizations for cardiac events
- Enhanced overall cardiovascular health
- Improved exercise capacity maintenance
EECP vs. Traditional Treatments: Comprehensive Comparison
| Treatment Aspect | EECP Therapy | Bypass Surgery | Stent Placement |
|---|---|---|---|
| Invasiveness | Completely non-invasive | Major surgical procedure | Minimally invasive |
| Recovery Time | No recovery needed | 6-12 weeks | 1-2 weeks |
| Hospital Stay | Outpatient treatment | 5-7 days | 1-2 days |
| Anesthesia Risk | None | General anesthesia required | Local/conscious sedation |
| Infection Risk | Zero | Surgical site infections possible | Catheter-related infections |
| Success Rate | 75-85% symptom improvement | 90-95% immediate success | 85-90% immediate success |
| Duration of Benefits | 3-5 years | 10-15 years | 1-3 years (restenosis risk) |
| Repeatability | Easily repeatable | Limited repeatability | Multiple procedures possible |
| Complication Rate | <1% | 2-5% | 1-3% |
| Mortality Risk | Virtually zero | 1-3% | <1% |
Advantages of EECP Over Conventional Approaches
The comparison reveals EECP therapy’s unique position in cardiac care. While surgical interventions may offer immediate mechanical relief, EECP provides a holistic approach that addresses underlying pathophysiology without associated surgical risks.
Key advantages include:
- Safety Profile: Exceptional safety record with minimal contraindications
- Quality of Life: Immediate return to normal activities during treatment
- Comprehensive Benefits: Addresses multiple aspects of cardiac dysfunction
- Patient Comfort: Pleasant, relaxing treatment experience
Who Needs EECP Therapy? Identifying Ideal Candidates
EECP therapy serves diverse patient populations, particularly those facing limitations with traditional treatments. When an angina patient doesn’t qualify for surgery or catheter-based coronary stenting, doctors may recommend EECP, highlighting its role as both alternative and complementary therapy.
Primary Candidates for EECP
Refractory Angina Patients: Individuals experiencing persistent chest pain despite optimal medical management represent ideal EECP candidates. These patients often face limited options and significant lifestyle restrictions.
High Surgical Risk Patients: Elderly patients or those with multiple comorbidities may not tolerate invasive procedures well. EECP offers therapeutic benefits without surgical risks.
Post-Surgical Patients: Individuals who have undergone previous cardiac procedures but continue experiencing symptoms benefit from EECP’s complementary effects.
Specific Clinical Indications
EECP therapy demonstrates efficacy across multiple cardiovascular conditions:
Chronic Stable Angina: Patients with effort-induced chest pain find significant relief through enhanced coronary perfusion.
Congestive Heart Failure: At least 90% of patients getting EECP have shown improvement in heart failure symptoms, including improved exercise tolerance and reduced hospitalizations.
Peripheral Vascular Disease: Enhanced circulation benefits extend beyond cardiac applications, improving peripheral blood flow.
Diabetic Cardiovascular Complications: Diabetic patients with microvascular disease experience improved perfusion and reduced complications.
EECP Treatment Protocol: What to Expect
Understanding the EECP treatment process helps patients prepare for this transformative therapy. The standard protocol involves 35 – 40 one-hour sessions scheduled over seven weeks, typically five days per week.
Session Structure and Experience
Each treatment session follows a carefully orchestrated protocol designed to maximize therapeutic benefits while ensuring patient comfort. Patients lie comfortably on a padded treatment table while pneumatic cuffs are positioned around their calves, lower thighs, and upper thighs.
Pre-treatment Assessment: Each session begins with vital sign monitoring and patient comfort evaluation.
Cuff Application: Specialized cuffs are positioned to ensure optimal compression distribution and patient comfort.
Treatment Delivery: Synchronized compression cycles are delivered based on individual cardiac rhythm patterns.
Post-treatment Monitoring: Patients are monitored for any immediate effects or concerns before discharge.
Treatment Environment and Patient Experience
The EECP treatment environment prioritizes patient comfort and relaxation. Many patients describe sessions as surprisingly pleasant, often reading, listening to music, or watching television during treatment. The gentle compression sensation is generally well-tolerated, with most patients finding it surprisingly comfortable.
Treatment centers typically provide:
- Comfortable, private treatment rooms
- Entertainment options during sessions
- Professional staff monitoring throughout treatment
- Flexible scheduling to accommodate patient needs
Lifestyle Integration: Holistic Approaches to Cardiac Health
EECP therapy’s effectiveness is enhanced through comprehensive lifestyle modifications that address cardiovascular risk factors. This integrated approach maximizes therapeutic outcomes while promoting long-term cardiac health.
Ayurvedic Principles in Cardiac Care
Ancient Ayurvedic wisdom offers valuable insights for modern cardiac care. Ayurvedic principles emphasize balance and natural healing, complementing EECP therapy’s non-invasive approach.
Rasayana Herbs: Adaptogenic herbs like Arjuna (Terminalia arjuna) have been traditionally used for cardiac support. Modern research validates their cardioprotective properties, making them valuable adjuncts to EECP therapy.
Pranayama Practices: Controlled breathing techniques enhance oxygen delivery and promote cardiac efficiency, synergizing with EECP’s circulation-enhancing effects.
Dietary Guidelines: Ayurvedic dietary principles emphasizing fresh, whole foods and avoiding processed substances support cardiovascular health during EECP treatment.
Homeopathic Support Systems
Homeopathic remedies can provide gentle support during EECP therapy, addressing individual constitutional needs and promoting overall healing responses.
Common homeopathic supports include:
- Crataegus: Often called the “heart tonic,” supporting cardiac muscle function
- Digitalis: For specific cardiac rhythm support under professional guidance
- Cactus Grandiflorus: Traditional use for chest pain and cardiac symptoms
Naturopathic Integration
Naturopathic medicine’s focus on treating root causes aligns perfectly with EECP therapy’s comprehensive approach. Naturopathic supports include:
Nutritional Optimization: Targeted supplementation with CoQ10, magnesium, and omega-3 fatty acids supports cardiac function and enhances EECP outcomes.
Herbal Medicine: Scientifically validated herbs like hawthorn (Crataegus species) provide cardiac support and may enhance treatment effectiveness.
Stress Management: Naturopathic stress reduction techniques complement EECP’s relaxing treatment environment.
Fasting and Intermittent Fasting Benefits
Controlled fasting protocols can significantly enhance EECP therapy outcomes by promoting cardiovascular health and reducing inflammatory markers.
Intermittent Fasting Protocols
Research demonstrates that properly implemented intermittent fasting can:
- Reduce inflammatory markers associated with atherosclerosis
- Improve insulin sensitivity and glucose metabolism
- Enhance autophagy processes that clear cellular debris
- Promote weight management and blood pressure reduction
16:8 Protocol: Eating within an 8-hour window and fasting for 16 hours daily provides sustainable benefits without extreme restrictions.
5:2 Approach: Normal eating five days per week with two days of reduced caloric intake offers flexibility while maintaining therapeutic benefits.
Fasting Safety Considerations
Fasting protocols should be implemented under professional supervision, especially for patients undergoing EECP therapy. Proper medical oversight ensures safety and maximizes benefits while avoiding potential complications.
Herbal Medicine and Nutraceutical Support
Evidence-based herbal medicines and targeted nutraceuticals can significantly enhance EECP therapy outcomes through multiple mechanisms of action.
Scientifically Validated Cardiac Herbs
Terminalia Arjuna: This Ayurvedic herb demonstrates remarkable cardioprotective properties through multiple mechanisms:
- Antioxidant activity reducing oxidative stress
- Anti-inflammatory effects on vascular endothelium
- Positive inotropic effects supporting cardiac contractility
- Lipid-lowering properties addressing atherosclerosis risk factors
Hawthorn (Crataegus species): Extensively researched for cardiac applications:
- Improved coronary circulation
- Enhanced cardiac output and exercise tolerance
- Antiarrhythmic properties
- Blood pressure regulation
Garlic (Allium sativum): Cardiovascular benefits include:
- Cholesterol reduction and atherosclerosis prevention
- Blood pressure lowering effects
- Antiplatelet activity reducing thrombosis risk
- Endothelial function improvement
Targeted Nutraceutical Support
Coenzyme Q10: Essential for cellular energy production, particularly important for cardiac muscle function. Supplementation supports:
- Mitochondrial energy production
- Antioxidant protection
- Blood pressure regulation
- Enhanced exercise tolerance
Magnesium: Critical mineral for cardiac function:
- Muscle relaxation and proper cardiac rhythm
- Blood pressure regulation
- Insulin sensitivity improvement
- Inflammation reduction
Omega-3 Fatty Acids: Essential for cardiovascular health:
- Anti-inflammatory effects
- Triglyceride reduction
- Improved endothelial function
- Reduced cardiac arrhythmia risk
Clinical Research and Evidence Base
EECP therapy’s effectiveness is supported by extensive clinical research spanning multiple decades and involving thousands of patients worldwide.
International Patient Registry Data
Data from the International Patient Registry demonstrate that EECP effectively decreased angina episodes and nitrate usage, and increased exercise tolerance in patients with refractory angina. This comprehensive registry provides real-world evidence of EECP’s therapeutic value across diverse patient populations.
Long-term Outcome Studies
The anti-ischemic benefits occur early and are sustained up to 5 years in patients, demonstrating the durability of EECP’s therapeutic effects. This longevity rivals and often exceeds the benefits of some invasive interventions.
Key research findings include:
- Significant reduction in angina frequency and severity
- Improved exercise tolerance and quality of life measures
- Reduced hospitalizations for cardiac events
- Enhanced cardiac function parameters
- Improved survival rates in specific patient populations
Mechanistic Studies
Advanced research techniques have elucidated EECP’s mechanisms of action:
- Enhanced coronary perfusion through diastolic augmentation
- Increased shear stress promoting endothelial function
- Angiogenic factor stimulation encouraging collateral formation
- Improved cardiac efficiency through afterload reduction
Safety Profile and Contraindications
EECP therapy’s exceptional safety profile makes it suitable for patients who may not tolerate invasive procedures. Serious adverse events are extremely rare, occurring in less than 1% of treated patients.
Absolute Contraindications
Certain conditions preclude EECP therapy:
- Severe aortic insufficiency
- Severe peripheral vascular disease affecting lower extremities
- Uncontrolled hypertension (>180/110 mmHg)
- Active phlebitis or deep vein thrombosis
- Pregnancy
Relative Contraindications
Some conditions require careful evaluation but may not exclude treatment:
- Moderate aortic insufficiency
- Severe chronic obstructive pulmonary disease
- Recent cardiac catheterization or surgery
- Bleeding disorders
Monitoring and Safety Protocols
Comprehensive safety protocols ensure patient wellbeing throughout treatment:
- Pre-treatment cardiovascular assessment
- Continuous monitoring during sessions
- Regular blood pressure and heart rate checks
- Patient comfort assessment and adjustment protocols
Integration with Conventional Medicine
EECP therapy works synergistically with conventional cardiac medications and treatments, often enhancing their effectiveness while potentially reducing required dosages.
Medication Interactions
EECP therapy generally has no negative interactions with cardiac medications. Many patients find they can reduce medication requirements under physician supervision as their symptoms improve.
Common medication categories that may be adjusted include:
- Antianginal medications (nitrates, beta-blockers)
- Blood pressure medications
- Cholesterol-lowering drugs
- Antiplatelet agents
Complementary Treatment Approaches
EECP therapy enhances rather than replaces appropriate medical management. Integration includes:
- Continued medical monitoring and adjustment
- Enhanced effectiveness of existing medications
- Reduced need for rescue medications
- Improved overall treatment outcomes
Nutritional Strategies for Enhanced Outcomes
Proper nutrition plays a crucial role in maximizing EECP therapy outcomes and promoting long-term cardiovascular health.
Anti-Inflammatory Nutrition
Chronic inflammation contributes significantly to cardiovascular disease progression. Anti-inflammatory nutrition strategies include:
Mediterranean Diet Principles: Emphasizing:
- High-quality olive oil and healthy fats
- Abundant vegetables and fruits
- Moderate fish consumption
- Limited processed foods
- Regular consumption of nuts and seeds
Specific Anti-Inflammatory Foods:
- Fatty fish rich in omega-3 fatty acids
- Leafy green vegetables high in nitrates
- Berries containing powerful antioxidants
- Turmeric and ginger for their anti-inflammatory compounds
- Green tea with protective polyphenols
Cardiac-Specific Nutrition
Certain nutrients specifically support cardiac function and enhance EECP outcomes:
Nitric Oxide Precursors: Foods rich in L-arginine and nitrates support endothelial function:
- Beets and beetroot juice
- Leafy green vegetables
- Watermelon and pomegranate
- Nuts and seeds
Antioxidant-Rich Foods: Protecting against oxidative stress:
- Colorful fruits and vegetables
- Dark chocolate (in moderation)
- Green tea and herbal teas
- Spices like turmeric and cinnamon
Patient Preparation and Optimization
Proper preparation enhances EECP therapy outcomes and ensures optimal patient experience throughout treatment.
Pre-Treatment Optimization
Medical Clearance: Comprehensive cardiovascular assessment ensures appropriateness for EECP therapy and identifies any necessary precautions.
Medication Review: Evaluation of current medications to optimize therapy and identify potential interactions or adjustments.
Lifestyle Assessment: Review of current diet, exercise, and lifestyle factors that may impact treatment outcomes.
During Treatment Optimization
Consistency: Regular attendance and session completion maximize therapeutic benefits.
Lifestyle Continuation: Maintaining healthy habits during treatment enhances outcomes.
Communication: Regular feedback to treatment providers ensures optimal comfort and effectiveness.
Post-Treatment Maintenance
Lifestyle Continuation: Maintaining healthy habits established during treatment sustains benefits.
Regular Monitoring: Periodic cardiovascular assessment tracks long-term outcomes.
Booster Treatments: Some patients benefit from periodic maintenance sessions to sustain improvements.
Future Directions and Emerging Research
EECP therapy continues evolving with advancing technology and expanding clinical applications.
Technological Advances
Enhanced Monitoring: Real-time hemodynamic monitoring during treatment allows for individualized optimization.
Portable Devices: Development of home-based EECP devices may expand accessibility and convenience.
Combined Therapies: Integration with other non-invasive treatments may enhance outcomes.
Expanding Applications
Research continues exploring EECP’s potential in various conditions:
- Peripheral vascular disease
- Diabetic complications
- Cognitive function enhancement
- Athletic performance optimization
Conclusion: The Future of Non-Surgical Cardiac Care
EECP therapy represents a paradigm shift in cardiovascular medicine, offering patients a safe, effective alternative to invasive procedures. The integration of this revolutionary treatment with holistic approaches including Ayurveda, naturopathy, herbal medicine, and targeted nutrition creates a comprehensive framework for cardiac health optimization.
The compelling evidence base, exceptional safety profile, and sustained therapeutic benefits position EECP therapy as a cornerstone of modern cardiac care. As healthcare systems worldwide grapple with increasing cardiovascular disease burden, non-invasive treatments like EECP offer hope for millions of patients seeking effective alternatives to bypass surgery and interventional procedures.
The future of cardiac care lies not just in technological advancement but in the integration of evidence-based non-invasive therapies that address both symptoms and underlying pathophysiology. EECP therapy, combined with comprehensive lifestyle interventions, represents this future today.
About the Author
Mr. Vivek Singh Sengar is a renowned clinical nutritionist, EECP trainer, and researcher with extensive expertise in treating lifestyle disorders and cardiovascular diseases. As the founder of FIT MY HEART and consultant at NEXIN HEALTH and MD CITY Hospital Noida, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar’s unique approach combines evidence-based EECP therapy with comprehensive nutritional interventions and lifestyle modifications. His research contributions have advanced understanding of EECP applications in various cardiovascular conditions. Through his practice at www.viveksengar.in, he continues to provide cutting-edge cardiac care while training the next generation of EECP practitioners.
His expertise spans clinical nutrition, cardiovascular disease management, diabetes care, and non-invasive cardiac therapies. Mr. Sengar’s commitment to patient-centered care and evidence-based medicine has established him as a leading authority in EECP therapy and lifestyle disease management.
💬 Need Expert Guidance for Your Health?
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Also Read: Ayurvedic Heart Blockage Treatment
Frequently Asked Questions: Non Surgical Heart Treatment
1. What is EECP therapy and how does it work? EECP (Enhanced External Counterpulsation) is an FDA-approved, non-invasive treatment that uses pneumatic cuffs on the legs to improve blood flow to the heart. The cuffs inflate and deflate in sync with the heartbeat, increasing oxygen delivery to the heart muscle and promoting the formation of natural bypass vessels.
2. Is EECP therapy safe and what are the side effects? EECP therapy has an exceptional safety profile with serious adverse events occurring in less than 1% of patients. Minor side effects may include temporary skin irritation from the cuffs or mild fatigue. The treatment is completely non-invasive with no anesthesia required.
3. How long does EECP treatment take and what is the typical protocol? Standard EECP therapy consists of 35 – 40 one-hour sessions scheduled over 7 weeks, typically 5 days per week. Each session is comfortable and relaxing, allowing patients to read, watch TV, or listen to music during treatment.
4. Who is a good candidate for EECP therapy? Ideal candidates include patients with chronic stable angina, those who are not candidates for surgery, patients with refractory symptoms despite optimal medical management, and individuals seeking non-invasive alternatives to bypass surgery or stenting.
5. How effective is EECP compared to bypass surgery or stenting? Research shows that over 75% of EECP patients experience significant reduction in angina symptoms. While bypass surgery may offer higher immediate success rates, EECP provides sustained benefits for 2-5 years without surgical risks or recovery time.
6. Can EECP therapy be combined with conventional medications? Yes, EECP therapy works synergistically with conventional cardiac medications and often enhances their effectiveness. Many patients can reduce medication requirements under physician supervision as their symptoms improve.
7. What lifestyle changes should I make during EECP treatment? Patients benefit from maintaining a heart-healthy diet, regular light exercise as tolerated, stress management techniques, and avoiding smoking. Anti-inflammatory nutrition and specific supplements may enhance treatment outcomes.
8. How soon will I see results from EECP therapy? Many patients begin experiencing symptom improvement within the first 2-3 weeks of treatment. Maximum benefits are typically achieved by completion of the full 35 – 40 session protocol, with continued improvement for several months afterward.
9. Is EECP therapy covered by insurance? EECP therapy is FDA-approved and covered by Medicare and many private insurance plans when medically indicated. Coverage varies by provider, so it’s important to verify benefits with your insurance company.
10. Can EECP therapy be repeated if symptoms return? Yes, EECP therapy can be safely repeated if symptoms recur after the initial treatment benefits diminish. Many patients undergo periodic maintenance treatments to sustain improvements.
11. What is the difference between EECP and other external counterpulsation therapies? EECP represents the most advanced form of external counterpulsation, with precise pneumatic control and FDA approval. It differs from older mechanical devices in its sophisticated timing and pressure control systems.
12. Are there any dietary restrictions during EECP treatment? There are no specific dietary restrictions, but patients are encouraged to follow a heart-healthy diet. Avoiding large meals immediately before treatment sessions can enhance comfort during therapy.
13. Can diabetic patients with heart disease benefit from EECP? Yes, diabetic patients often experience significant benefits from EECP therapy, including improved circulation, reduced cardiac symptoms, and enhanced overall cardiovascular health. The therapy may also help with diabetic complications.
14. How does EECP therapy promote natural bypass formation? EECP stimulates the release of angiogenic factors that promote the growth of collateral blood vessels around blocked arteries. This natural bypass formation provides long-term improvement in heart muscle blood supply.
15. What should I expect during my first EECP session? Your first session will include a comprehensive evaluation, cuff fitting, and gradual introduction to the treatment pressure. The medical team will ensure your comfort and explain the process throughout the session. Most patients find the experience surprisingly pleasant and relaxing.
