Non-Surgical Treatment of Heart Blockages: Heart blockages no longer mean you must accept the risks of surgery or live with limiting symptoms. Revolutionary non-surgical treatments have transformed how we approach coronary artery disease, offering hope to millions worldwide. The integration of Enhanced External Counterpulsation (EECP) with holistic healing modalities presents a comprehensive solution that addresses both symptoms and root causes.
Traditional cardiac interventions often focus on mechanical solutions without addressing underlying metabolic imbalances. Today’s integrated approach combines cutting-edge technology with time-tested natural therapies to promote genuine cardiovascular healing. This comprehensive strategy offers patients safer alternatives while achieving remarkable clinical outcomes.
Modern cardiology increasingly recognizes that heart blockages develop through complex interactions of lifestyle, genetics, and environmental factors. Addressing these multiple pathways requires multi-modal treatment approaches that go beyond conventional medical interventions. The integration of EECP therapy with Ayurvedic medicine, nutritional interventions, and lifestyle modifications represents the future of cardiac care.
Global Statistics of Heart Blockages and Long-Term Impact
Coronary artery disease affects over 200 million people globally, making it the leading cause of death worldwide. Heart failure is a serious global health problem, and coronary artery disease is one of the main causes. The economic burden exceeds $200 billion annually in healthcare costs alone, not including lost productivity and quality of life impacts.
Statistical analysis reveals that 85% of heart attacks occur due to plaque rupture in arteries with less than 70% blockage. This finding revolutionizes our understanding of coronary artery disease progression and highlights the importance of comprehensive treatment approaches that address plaque stability rather than just blockage severity.
Mortality rates from coronary artery disease have declined in developed countries due to better prevention and treatment strategies. However, developing nations experience increasing rates as lifestyle-related risk factors become more prevalent. India alone accounts for nearly 25% of global cardiovascular deaths, with heart disease affecting younger populations compared to Western countries.
Long-term consequences extend beyond immediate cardiac events. Patients with coronary artery disease experience 40% higher rates of depression, cognitive decline, and reduced life expectancy. Quality of life measures consistently show significant impairment in physical, emotional, and social functioning. These comprehensive impacts necessitate treatment approaches that address the whole person rather than just the blocked arteries.
Understanding Heart Blockages: Pathogenesis and Clinical Pathways
Coronary artery blockages develop through a complex process called atherosclerosis, involving multiple cellular and molecular pathways. Understanding these mechanisms helps explain why integrated treatment approaches often achieve superior outcomes compared to single-intervention strategies.
Atherosclerotic Process Development
Endothelial dysfunction represents the earliest stage of blockage formation. Inflammatory mediators, oxidative stress, and metabolic imbalances damage the inner arterial lining, creating sites for plaque accumulation. This process begins decades before symptoms appear, emphasizing the importance of early intervention strategies.
Lipid accumulation follows endothelial injury as modified cholesterol particles penetrate arterial walls. Immune system activation occurs as macrophages attempt to clear these lipids, transforming into foam cells that promote further inflammation. This inflammatory cascade perpetuates plaque growth and instability.
Plaque composition determines clinical outcomes more than blockage severity. Stable plaques with thick fibrous caps rarely cause heart attacks, while unstable plaques with thin caps and large lipid cores frequently rupture, causing acute coronary events. This understanding explains why comprehensive treatment approaches focus on plaque stabilization.
Clinical Progression Patterns
Early stages of coronary artery disease remain asymptomatic as collateral circulation develops to compensate for reduced blood flow. The heart’s remarkable ability to adapt masks the underlying problem until blockages become severe or multiple vessels are affected.
Stable angina develops when oxygen demand exceeds supply during physical exertion or emotional stress. This predictable pattern of chest discomfort serves as a warning sign that coronary circulation is compromised. Recognition of stable angina patterns allows for timely intervention before more serious complications develop.
Acute coronary syndromes occur when unstable plaques rupture, causing sudden arterial occlusion. These events can happen in arteries with minimal prior blockage, highlighting the importance of comprehensive risk factor management rather than focusing solely on known blockages.
Enhanced External Counterpulsation: The Foundation of Non-Surgical Treatment
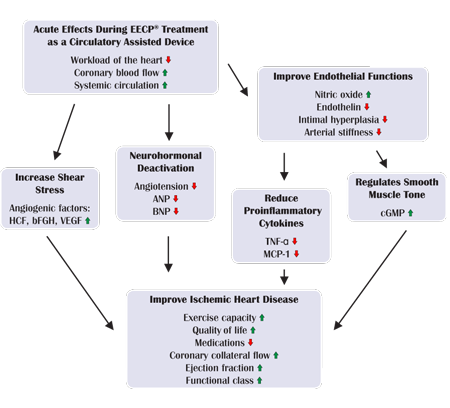
EECP treatment applies pressure to blood vessels in your lower limbs. The pressure increases blood flow back to your heart, so your heart works better. This innovative therapy represents the cornerstone of non-surgical heart blockage treatment, offering profound benefits through multiple physiological mechanisms.
EECP Mechanism of Action
Synchronized pneumatic compression of the lower extremities creates a secondary circulation system that dramatically improves cardiac hemodynamics. During diastole, sequential cuff inflation enhances coronary perfusion pressure by up to 40%, delivering crucial oxygen and nutrients to oxygen-starved heart muscle.
Afterload reduction occurs during systole as cuffs rapidly deflate, creating a vacuum effect that reduces the resistance against which the heart must pump. This dual mechanism of enhanced perfusion and reduced workload addresses the fundamental problems in coronary artery disease.
Collateral circulation development represents one of EECP’s most significant long-term benefits. Enhanced shear stress stimulates growth factor release, promoting new blood vessel formation around blocked arteries. These natural bypass vessels can restore near-normal blood flow to previously compromised areas.
Physiological Benefits of EECP
Coronary perfusion improvements occur immediately during EECP treatment and continue developing over weeks to months. Patients often experience symptom relief within the first few sessions as enhanced oxygen delivery reaches previously ischemic heart muscle. Long-term benefits result from structural improvements in coronary circulation.
Cardiac efficiency gains occur through improved preload optimization and afterload reduction. The failing heart works more efficiently when these hemodynamic parameters are optimized. Energy conservation allows the heart to perform better while consuming less oxygen, breaking the cycle of ischemia and dysfunction.
Neurohormonal modulation through EECP helps normalize the pathological changes that perpetuate heart disease. Reduced sympathetic nervous system activation and improved baroreceptor function contribute to blood pressure normalization and reduced arrhythmia risk.
Ayurvedic Approaches to Heart Blockage Reversal
Charaka introduced ten drugs under Hridya Mahakashaya group for treating heart diseases, establishing Ayurveda’s sophisticated understanding of cardiovascular health. Modern research validates many traditional Ayurvedic principles for treating coronary artery disease through natural methods.
Classical Ayurvedic Understanding
Ayurvedic texts describe heart blockages as manifestations of Vata dosha imbalance affecting circulation channels (srotas). This ancient understanding aligns remarkably with modern concepts of endothelial dysfunction and inflammatory processes in atherosclerosis development.
Tridoshic imbalance creates the foundation for cardiovascular disease according to Ayurvedic principles. Vata governs circulation, Pitta manages metabolic processes, and Kapha provides structural support. Restoring balance among these fundamental energies promotes natural healing of blocked arteries.
Agni (digestive fire) dysfunction contributes to toxin accumulation (ama) that blocks circulation channels. Improving digestive capacity through specific herbs and dietary practices helps eliminate existing blockages while preventing new ones from forming.
Proven Ayurvedic Herbs for Heart Health
Arjuna (Terminalia arjuna) stands as the premier Ayurvedic cardiac herb, extensively researched for its cardioprotective properties. Herbal remedies such as Arjuna, Ashwagandha, Guggulu, curcumin, Triphala and many other combination of herbs is used in Ayurveda to support heart health. Clinical studies demonstrate Arjuna’s ability to improve cardiac function, reduce cholesterol, and enhance exercise tolerance.
Guggulu (Commiphora mukul) provides powerful lipid-lowering effects while reducing inflammation throughout the cardiovascular system. Research shows significant improvements in cholesterol profiles and arterial flexibility with regular Guggulu supplementation.
Ashwagandha (Withania somnifera) addresses the stress component of heart disease through its adaptogenic properties. Chronic stress contributes significantly to cardiovascular disease progression, making stress management essential for comprehensive treatment.
Hawthorn (Crataegus species) strengthens heart muscle contractions while improving coronary circulation. European studies demonstrate significant improvements in heart failure symptoms and exercise capacity with Hawthorn supplementation.
Ayurvedic Treatment Protocols
Panchakarma detoxification plays a crucial role in removing accumulated toxins that contribute to arterial blockages. Specific procedures like Virechana (therapeutic purgation) and Basti (medicated enemas) help eliminate deep-seated toxins while rejuvenating cardiovascular tissues.
Rasayana therapy focuses on cellular regeneration and tissue repair. Specialized formulations containing gold preparations (Swarna Bhasma) and processed minerals enhance cardiac muscle strength and coronary circulation when administered under expert guidance.
Lifestyle modifications form the foundation of Ayurvedic cardiac care. Daily routines aligned with natural circadian rhythms, appropriate exercise, and stress management techniques support the healing process initiated by herbal medicines and detoxification procedures.
Integrative Nutritional Strategies for Blockage Reversal
Evidence-based nutrition plays a pivotal role in reversing heart blockages through multiple mechanisms including inflammation reduction, lipid optimization, and endothelial function improvement. The integration of modern nutritional science with traditional dietary wisdom creates powerful healing protocols.
Anti-Inflammatory Nutrition
Omega-3 fatty acids from marine sources provide potent anti-inflammatory effects that stabilize arterial plaques and reduce cardiovascular events. Research demonstrates 30-40% reduction in cardiac death rates with adequate omega-3 intake from food sources or high-quality supplements.
Polyphenol-rich foods including berries, green tea, and dark chocolate provide antioxidant protection while improving endothelial function. These compounds help reverse the oxidative damage that initiates and perpetuates atherosclerotic plaque formation.
Mediterranean dietary patterns consistently show superior outcomes for cardiovascular health in large population studies. The combination of healthy fats, antioxidant-rich vegetables, and moderate amounts of lean protein provides optimal nutrition for arterial healing.
Targeted Nutrient Protocols
Magnesium deficiency affects over 80% of heart disease patients, contributing to arterial spasm, rhythm disturbances, and blood pressure elevation. Optimal magnesium status requires 400-800mg daily from food sources and supplements combined.
Vitamin K2 directs calcium away from arterial walls and into bones where it belongs. Research shows significant reduction in coronary artery calcification with adequate K2 intake, particularly the MK-7 form found in fermented foods.
Coenzyme Q10 supports cellular energy production in heart muscle while providing antioxidant protection. Patients taking statin medications require CoQ10 supplementation to prevent deficiency-related muscle weakness and cardiac complications.
Intermittent Fasting and Metabolic Optimization
Time-restricted eating patterns promote autophagy, the cellular cleaning process that removes damaged proteins and organelles. This natural detoxification mechanism helps clear arterial plaques while improving overall cardiovascular health.
Ketogenic approaches can rapidly improve insulin sensitivity and reduce inflammatory markers in appropriately selected patients. However, these dietary changes require professional supervision to ensure safety and effectiveness, particularly in patients with existing heart disease.
Nutrient timing strategies optimize the body’s natural healing processes. Consuming anti-inflammatory foods during periods of peak absorption and avoiding pro-inflammatory foods during vulnerable periods enhances treatment effectiveness.
Lifestyle Modifications and Natural Healing Practices
Comprehensive lifestyle transformation addresses the root causes of heart blockages while supporting the healing effects of medical interventions. These changes often produce more profound long-term benefits than medical treatments alone.
Exercise and Movement Therapy
Graduated exercise programs safely improve cardiovascular fitness in patients with heart blockages. Starting with low-intensity activities and progressively increasing duration and intensity promotes collateral circulation development while strengthening heart muscle.
Yoga and Tai Chi provide gentle cardiovascular conditioning while incorporating stress reduction techniques. These mind-body practices improve flexibility, balance, and cardiac efficiency while reducing the psychological stress that contributes to heart disease progression.
Resistance training, when appropriately prescribed, enhances overall cardiovascular health by improving insulin sensitivity and muscle mass. Progressive resistance exercises should be initiated under professional guidance to ensure safety in patients with known coronary artery disease.
Stress Management and Mental Health
Chronic stress contributes significantly to heart disease through multiple pathways including inflammation, blood pressure elevation, and unhealthy coping behaviors. Comprehensive stress management becomes essential for optimal cardiovascular health.
Meditation practices consistently demonstrate cardiovascular benefits in clinical studies. Regular meditation practice can reduce blood pressure, improve heart rate variability, and decrease stress hormone levels that contribute to arterial damage.
Sleep optimization plays a crucial role in cardiovascular recovery. Quality sleep supports immune function, hormone balance, and cellular repair processes essential for arterial healing. Most adults require 7-9 hours of quality sleep for optimal cardiovascular health.
Homeopathic and Naturopathic Interventions
Homeopathic medicine offers individualized treatment approaches that address the unique symptom patterns of each patient with heart blockages. While controversial in mainstream medicine, many patients report significant improvements with properly prescribed homeopathic remedies.
Constitutional Homeopathic Treatment
Aconitum napellus addresses acute anxiety and panic associated with heart conditions, particularly when symptoms develop suddenly after emotional shock or stress. This remedy helps calm the nervous system response that can worsen cardiac symptoms.
Arsenicum album benefits patients with heart blockages who experience anxiety, restlessness, and fatigue. The remedy addresses the fear and worry that often accompany cardiovascular disease while supporting overall vitality.
Crataegus oxyacantha in homeopathic potencies complements the herbal form by addressing functional heart complaints and supporting cardiac muscle strength. This remedy helps optimize heart function at the energetic level.
Naturopathic Detoxification
Chelation therapy, when appropriately administered, may help remove heavy metals that contribute to cardiovascular disease. Some studies suggest benefits for coronary artery disease, though this remains controversial in mainstream cardiology.
Lymphatic drainage techniques support the body’s natural detoxification processes while improving circulation. Manual lymphatic drainage and specific herbal protocols enhance toxin elimination through multiple pathways.
Hydrotherapy applications including contrast showers and constitutional hydrotherapy stimulate circulation while supporting immune function. These simple techniques can be incorporated into daily routines to support cardiovascular health.
Non-Surgical Treatment of Heart Blockages: Integrated Protocol Design
Successful treatment of heart blockages requires careful integration of multiple therapeutic modalities tailored to individual patient needs. The synergistic effects of combined approaches often exceed the benefits of any single intervention.
Treatment Sequencing and Timing
Initial stabilization focuses on symptom relief and risk reduction through EECP therapy combined with basic lifestyle modifications. This foundation provides immediate benefits while preparing patients for more comprehensive interventions.
Detoxification phases incorporate Ayurvedic panchakarma, nutritional protocols, and naturopathic drainage techniques to remove accumulated toxins that contribute to arterial blockages. Proper detoxification enhances the effectiveness of subsequent healing interventions.
Regenerative phases emphasize tissue repair and functional improvement through targeted nutrition, herbal medicines, and continued EECP therapy. This phase requires patient commitment to comprehensive lifestyle changes for optimal outcomes.
Individualized Treatment Plans
Patient assessment includes comprehensive evaluation of constitution, current symptoms, lifestyle factors, and treatment preferences. This holistic assessment guides the selection and sequencing of therapeutic interventions.
Monitoring protocols track both objective measures (blood pressure, lipid levels, exercise tolerance) and subjective improvements (symptom relief, energy levels, quality of life). Regular assessment allows for treatment plan modifications based on patient response.
Long-term maintenance strategies ensure sustained benefits while preventing disease progression. Most patients require ongoing support through periodic EECP treatments, continued lifestyle modifications, and regular monitoring.
Comparison: Integrated Non-Surgical vs. Conventional Treatment Approaches
| Treatment Parameter | Integrated Non-Surgical | Angioplasty/Stents | Bypass Surgery | Medication Only |
|---|---|---|---|---|
| Invasiveness | Non-invasive | Minimally invasive | Highly invasive | Non-invasive |
| Hospital Stay | Outpatient | 1-2 days | 5-10 days | Outpatient |
| Recovery Time | Immediate | 1-2 weeks | 6-12 weeks | Immediate |
| Success Rate | 75-85% | 85-95% | 90-95% | 60-70% |
| Complication Risk | <1% | 3-5% | 8-15% | 10-20% |
| Long-term Benefits | 3-7 years | 5-10 years | 10-20 years | Ongoing |
| Address Root Causes | Yes | No | No | Partially |
| Quality of Life | Excellent | Good | Good | Variable |
| Repeat Procedures | Yes (safe) | Yes (limited) | Yes (high risk) | N/A |
| Natural Healing | Promotes | Prevents | Prevents | Neutral |
Advantages of Integrated Approach
Comprehensive healing addresses multiple disease pathways simultaneously, often achieving superior long-term outcomes compared to single-intervention strategies. Patients experience improvements in overall health and vitality beyond just cardiac symptoms.
Safety profiles favor integrated non-surgical approaches for many patients, particularly those with multiple comorbidities or advanced age. The minimal risk profile allows treatment of patients who might not be candidates for invasive procedures.
Sustainability of benefits often exceeds conventional treatments because integrated approaches address root causes rather than just symptoms. Patients maintain improvements through lifestyle changes and periodic maintenance treatments.
Limitations and Considerations
Treatment duration for integrated approaches typically requires months rather than the immediate results possible with surgical interventions. Patients must commit to comprehensive lifestyle changes for optimal outcomes.
Severe blockages may still require conventional interventions as initial stabilization before implementing integrated approaches. Emergency situations necessitate immediate medical intervention regardless of patient preferences for natural treatments.
Individual variation in response to integrated treatments requires personalized approaches and may involve trial periods to determine optimal treatment combinations. Patient commitment and compliance significantly influence treatment outcomes.
Who Needs Integrated Non-Surgical Treatment for Heart Blockages?
Understanding appropriate candidates for integrated non-surgical treatment helps optimize patient selection and treatment outcomes. Multiple factors influence candidacy for this comprehensive approach.
Primary Candidates
Patients with stable coronary artery disease experiencing limiting symptoms despite optimal medical management represent ideal candidates for integrated treatment. Non-Surgical Candidates: People who are not candidates for invasive procedures due to age, comorbidities, or other health risks may consider EECP therapy as a safer alternative.
Individuals seeking alternatives to invasive procedures find integrated approaches particularly attractive. Personal preferences for natural healing modalities and concerns about surgical risks motivate many patients to explore comprehensive non-surgical treatment options.
Those with multiple vessel disease or diffuse coronary artery involvement may benefit from integrated approaches that address global cardiac perfusion rather than focal interventions. The comprehensive nature of integrated treatment can improve overall cardiac function.
Clinical Indications
Chronic stable angina that limits daily activities provides clear indication for integrated treatment. Patients experiencing chest discomfort, shortness of breath, or fatigue with minimal exertion often achieve dramatic improvements with comprehensive therapy.
Heart failure symptoms in patients with ischemic cardiomyopathy benefit from the hemodynamic improvements provided by EECP combined with supportive natural therapies. Improved cardiac efficiency can reduce symptoms and enhance quality of life.
Refractory symptoms despite optimal conventional treatment indicate the need for alternative approaches. Patients who continue experiencing limitations after maximum medical therapy may find significant relief through integrated treatment protocols.
Contraindications and Precautions
Absolute contraindications include severe valvular disease, active bleeding disorders, and severe peripheral vascular disease that would interfere with EECP therapy. These conditions require conventional medical management before considering integrated approaches.
Relative contraindications require individual assessment and may include pregnancy, severe hypertension, and certain arrhythmias. Careful risk-benefit analysis guides treatment decisions in these situations.
Patient motivation and compliance represent crucial factors in treatment success. Integrated approaches require significant lifestyle changes and treatment commitment that not all patients can sustain successfully.
Monitoring and Outcome Assessment
Comprehensive monitoring ensures treatment safety and effectiveness while allowing for protocol modifications based on patient response. Multiple assessment parameters provide a complete picture of treatment progress.
Objective Measures
Exercise tolerance testing provides quantifiable measures of functional improvement throughout treatment. Progressive increases in exercise duration and intensity indicate successful treatment response and guide activity recommendations.
Cardiac imaging studies including echocardiography and nuclear perfusion scans can demonstrate improvements in cardiac function and blood flow patterns. These objective measures support subjective symptom improvements and guide treatment decisions.
Laboratory parameters including lipid profiles, inflammatory markers, and cardiac enzymes help track metabolic improvements and cardiovascular risk reduction. Regular monitoring ensures treatment safety and effectiveness.
Subjective Assessment
Symptom questionnaires track changes in chest discomfort, shortness of breath, fatigue, and exercise limitations. Standardized instruments provide reliable measures of symptom improvement over time.
Quality of life assessments encompass physical, emotional, and social functioning domains. Improvements in these areas often represent the most meaningful outcomes for patients receiving integrated treatment.
Patient satisfaction measures help assess treatment acceptance and identify areas for protocol improvement. High satisfaction rates support continued treatment compliance and positive outcomes.
Long-term Follow-up
Sustained benefit assessment requires follow-up extending years beyond initial treatment. Most patients maintain improvements for 3-5 years after comprehensive integrated treatment programs.
Risk factor monitoring ensures continued optimization of cardiovascular health through lifestyle maintenance and periodic treatment updates. Regular assessment prevents disease progression and maintains treatment benefits.
Treatment modification protocols allow for adjustments based on changing patient needs and treatment response. Flexibility in treatment approaches optimizes long-term outcomes and patient satisfaction.
Future Directions in Integrated Cardiac Care
Emerging technologies and treatment modalities continue expanding options for non-surgical treatment of heart blockages. These developments promise enhanced effectiveness and broader applicability of integrated approaches.
Technological Advances
Enhanced EECP devices with improved monitoring capabilities and treatment customization options are being developed. Real-time hemodynamic feedback may allow for more precise treatment optimization and improved outcomes.
Telemedicine integration enables remote monitoring and treatment adjustments, making integrated care more accessible to patients in remote locations. Digital health platforms can support lifestyle modifications and treatment compliance.
Artificial intelligence applications may help predict treatment response and optimize protocol selection based on individual patient characteristics. Machine learning algorithms could enhance treatment personalization and outcome prediction.
Research Developments
Mechanistic studies continue elucidating the cellular and molecular mechanisms underlying integrated treatment benefits. Better understanding of treatment mechanisms will guide protocol optimization and patient selection.
Combination therapy trials are investigating optimal integration of various treatment modalities. These studies will establish evidence-based protocols for comprehensive cardiovascular care.
Long-term outcome studies will provide crucial data about treatment durability and optimal maintenance protocols. Extended follow-up data will support broader adoption of integrated treatment approaches.
Conclusion: Transforming Cardiovascular Care Through Integration
The integration of EECP therapy with holistic healing modalities represents a paradigm shift toward comprehensive, patient-centered cardiovascular care. This approach addresses the complex, multifactorial nature of heart blockages while minimizing treatment risks and maximizing patient comfort.
Evidence supporting integrated non-surgical treatment continues growing as research demonstrates sustained benefits and excellent safety profiles. Patients who might not be candidates for conventional interventions now have access to effective treatment options that can dramatically improve their quality of life and long-term prognosis.
Success with integrated treatment requires commitment to comprehensive lifestyle changes and ongoing therapeutic support. However, the profound improvements in symptoms, functional capacity, and overall well-being achieved through these approaches justify the required commitment for most patients.
The future of cardiovascular medicine lies in personalized, integrated approaches that address individual patient needs while promoting natural healing processes. As evidence continues accumulating and technologies advance, integrated non-surgical treatment will likely become standard care for many patients with coronary artery disease.
Healthcare providers increasingly recognize that optimal cardiovascular care requires addressing lifestyle factors, stress management, and underlying metabolic imbalances alongside medical interventions. Integrated approaches provide the comprehensive framework necessary for achieving these multifaceted treatment goals.
Patients seeking alternatives to invasive cardiac procedures can find hope and healing through evidence-based integrated treatment protocols. The combination of advanced medical technology with time-tested natural healing modalities offers the best of both approaches while minimizing risks and maximizing benefits.
About the Author
Mr. Vivek Singh Sengar is a pioneering clinical nutritionist and researcher specializing in EECP Therapy and Clinical Nutrition. With extensive experience treating lifestyle disorders, he has successfully managed over 25,000 patients with heart disease and diabetes across the globe.
As the Founder of FIT MY HEART and a Consultant at NEXIN HEALTH and MD CITY Hospital Noida, Mr. Sengar has developed innovative integrated treatment protocols that combine advanced medical technology with evidence-based natural therapies. His comprehensive approach to cardiovascular care has helped countless patients avoid invasive procedures while achieving remarkable clinical improvements.
Mr. Sengar’s research contributions focus on the integration of EECP therapy with nutritional interventions and lifestyle modifications. His work demonstrates how comprehensive treatment approaches can address the root causes of cardiovascular disease while promoting sustainable health improvements.
Committed to patient education and empowerment, Mr. Sengar provides personalized treatment plans that honor individual preferences while maintaining scientific rigor. His integrated approach to cardiovascular care represents the future of personalized medicine.
For comprehensive cardiac care and personalized treatment consultations, visit www.viveksengar.in or contact his practice to explore how integrated non-surgical treatments can transform your cardiovascular health.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurverdic Heart Blockage Treatment
Revolutionary Non Surgical Heart Treatment
Frequently Asked Questions (FAQs)
1. What is EECP therapy and how does it help treat heart blockages without surgery?
Enhanced External Counterpulsation (EECP) is a non-invasive treatment that uses pneumatic cuffs wrapped around your legs to improve blood flow to the heart. The cuffs inflate and deflate in sync with your heartbeat, increasing blood flow to coronary arteries by up to 40% while reducing the heart’s workload. This dual action helps develop natural bypass vessels around blocked arteries, providing long-term symptom relief without surgical intervention.
2. How effective is integrated non-surgical treatment compared to angioplasty or bypass surgery?
Integrated non-surgical approaches show 75-85% success rates with less than 1% complication risk, compared to surgical options with 85-95% success but higher complication rates (3-15%). While immediate results may favor surgery, integrated treatments address root causes and often provide longer-lasting benefits (3-7 years) with the ability for safe repeat treatments when needed.
3. Can Ayurvedic herbs really reverse heart blockages naturally?
Research validates several Ayurvedic herbs for cardiovascular health. Arjuna (Terminalia arjuna) has been clinically proven to improve cardiac function and reduce cholesterol. Guggulu provides significant lipid-lowering effects, while Ashwagandha addresses stress-related heart disease factors. These herbs work synergistically to reduce inflammation, improve circulation, and support natural healing processes that can help stabilize and potentially reverse arterial blockages.
4. Who is a good candidate for non-surgical heart blockage treatment?
Ideal candidates include patients with stable coronary artery disease experiencing limiting symptoms, those seeking alternatives to invasive procedures, individuals with multiple vessel disease, and patients who are high-risk surgical candidates due to age or comorbidities. People with chronic stable angina, heart failure symptoms, or refractory symptoms despite optimal medical treatment often benefit significantly from integrated approaches.
5. What lifestyle changes are essential for reversing heart blockages naturally?
Key lifestyle modifications include adopting an anti-inflammatory Mediterranean-style diet rich in omega-3 fatty acids, implementing regular graduated exercise programs, practicing stress management through meditation or yoga, optimizing sleep quality (7-9 hours nightly), and eliminating smoking. Intermittent fasting and targeted nutritional supplementation with magnesium, vitamin K2, and CoQ10 also support arterial healing processes.
6. How long does EECP treatment take and what can I expect during sessions?
Standard EECP treatment involves 35 one-hour sessions over 5-7 weeks. During each session, you lie comfortably while pneumatic cuffs on your legs inflate and deflate synchronized with your heartbeat. Most patients find the treatment relaxing and can read or listen to music. Many experience symptom improvement within the first few sessions, with continued benefits developing over the treatment course.
7. Are there any side effects or risks with integrated non-surgical treatment?
Integrated non-surgical treatments have excellent safety profiles with minimal side effects. EECP may cause minor leg discomfort or skin irritation in less than 5% of patients. Ayurvedic herbs are generally well-tolerated when properly prescribed, though individual sensitivities can occur. Nutritional changes may cause temporary digestive adjustments. Serious adverse events are extremely rare (<0.1%) with proper supervision.
8. Can I combine EECP with my current heart medications?
Yes, EECP therapy is designed to complement existing cardiac medications, not replace them. Most patients continue their prescribed medications during EECP treatment. The therapy may actually enhance medication effectiveness by improving drug delivery to heart tissues. However, medication adjustments may be needed as symptoms improve, so regular monitoring with your cardiologist is essential.
9. How much does integrated non-surgical heart treatment cost compared to surgery?
While specific costs vary by location and treatment components, integrated non-surgical approaches are typically more cost-effective than surgical interventions. EECP treatment eliminates hospitalization costs, surgical fees, and complication management expenses. Many insurance plans cover EECP therapy for appropriate candidates. The long-term cost benefits include reduced hospitalizations and improved quality of life.
10. What role does stress management play in reversing heart blockages?
Chronic stress significantly contributes to heart disease through inflammation, blood pressure elevation, and unhealthy behaviors. Stress hormones directly damage arterial walls and promote plaque formation. Effective stress management through meditation, yoga, adequate sleep, and lifestyle balance can reduce cardiovascular risk by 30-40%. Integrated treatment programs emphasize stress reduction as essential for optimal outcomes.
11. Can fasting help reverse heart blockages, and what type is recommended?
Intermittent fasting can support heart health by promoting autophagy (cellular cleaning), improving insulin sensitivity, and reducing inflammation. Time-restricted eating (12-16 hour fasts) is generally safe and effective for most heart patients. However, fasting protocols should be supervised by healthcare professionals, especially for patients with diabetes or on cardiac medications, as adjustments may be needed.
12. How do I know if the integrated treatment is working for my heart blockages?
Treatment effectiveness can be measured through both subjective and objective improvements. Subjectively, you may notice reduced chest discomfort, improved exercise tolerance, increased energy levels, and better sleep quality. Objective measures include improved exercise stress test results, better echocardiogram findings, normalized blood pressure, and improved lipid profiles. Most patients notice improvements within 2-4 weeks of starting treatment.
13. Is integrated non-surgical treatment suitable for severe heart blockages (90%+ blockage)?
Severe blockages may require initial conventional intervention for stabilization, followed by integrated approaches for long-term management and prevention. However, some patients with severe blockages who are not surgical candidates have achieved significant symptom relief through comprehensive integrated treatment. Individual assessment by qualified practitioners is essential to determine the most appropriate treatment sequence.
14. What is the success rate for avoiding future heart attacks with integrated treatment?
Integrated approaches that address root causes often provide superior long-term protection compared to treatments focusing only on blockages. Research shows 30-50% reduction in future cardiac events when comprehensive lifestyle modifications are combined with appropriate medical interventions. Success depends on patient commitment to lifestyle changes and regular follow-up care.
15. Can I do EECP treatment if I have other health conditions like diabetes or high blood pressure?
EECP is generally safe for patients with diabetes and well-controlled high blood pressure. In fact, these conditions often improve during treatment due to enhanced circulation and reduced cardiac workload. However, certain conditions like severe peripheral vascular disease, active bleeding disorders, or severe aortic valve problems may be contraindications. Comprehensive evaluation ensures treatment safety and appropriateness for each individual.
References
- Enhanced External Counterpulsation in Ischemic Heart Failure: A Systematic Review. Current Cardiology Reports, 2023.
- Cleveland Clinic. Enhanced External Counterpulsation (EECP). Medical Information, 2024.
- Credential evidences of Ayurvedic cardio-vascular herbs. PMC, National Center for Biotechnology Information.
- A Prospective Trial of Ayurveda for Coronary Heart Disease: A Pilot Study. PubMed, 2015.
- Ayurvedic Treatment for Coronary Artery Disease. Planet Ayurveda, 2024.
- Natural Ayurvedic Solutions for Reversing Heart Blockage. HIIMS Hospital, 2024.
- University of Michigan Health. EECP Treatment Patient Information, 2024.
- Flow Therapy for Heart Conditions. Flow Therapy Centers, 2024.
- American Heart Association. Heart Disease and Stroke Statistics, 2024.
- European Society of Cardiology. Guidelines for Chronic Coronary Syndromes, 2023.