What is Pancreatitis: Pancreatitis is inflammation of the pancreas, a vital organ responsible for producing digestive enzymes and hormones like insulin. This condition can range from mild to severe and life-threatening. In this comprehensive blog, we will explore pancreatitis in detail – its types, causes, symptoms, treatment options, and how it can be effectively managed.
Types of Pancreatitis
Pancreatitis primarily comes in two forms:
1. Acute Pancreatitis
- Sudden inflammation that can last from a few days to several weeks
- 80% of cases have mild symptoms and recover completely
- 20% of cases can be severe, leading to complications like organ failure and infections
2. Chronic Pancreatitis
- Long-lasting inflammation that causes permanent damage to the pancreas
- Usually develops gradually over many years
- Can cause permanent loss of pancreatic function, leading to diabetes and digestive problems
Global Statistics
Pancreatitis represents a significant health concern worldwide:
- Globally, the incidence of acute pancreatitis ranges between 13-45 per 100,000 people
- In India, it occurs at a rate of approximately 6-7 cases per 100,000 people, but this is increasing
- Men are more affected than women, especially in chronic pancreatitis
- Higher cases are observed in urban areas
- In India, alcohol consumption and gallstones are the leading causes of pancreatitis
Global Statistics on Pancreatitis
-
Every year, around 3 to 5 million people globally suffer from Acute Pancreatitis.
-
According to WHO, patients with Chronic Pancreatitis often experience 40% or more digestive complications.
-
In India, alcohol, high-fat diet, and gallstones are among the top causes.
Causes of Pancreatitis
Major Causes of Acute Pancreatitis:
- Gallstones – The most common cause in India (40-50% of cases)
- Excessive Alcohol Consumption – The second most common cause (30-35% of cases)
- Medication Side Effects – Certain antibiotics, immunosuppressants, and painkillers
- Hypertriglyceridemia – High levels of triglycerides in the blood
- Hypercalcemia – High levels of calcium in the blood
- Pancreatic Tumors
- Post-procedural – Following procedures like ERCP (Endoscopic Retrograde Cholangiopancreatography)
- Genetic Causes
- Autoimmune Diseases
- Infections – Certain viral infections like mumps
Major Causes of Chronic Pancreatitis:
- Long-term Alcohol Abuse – In approximately 70% of cases
- Genetic Causes – Particularly mutations in PRSS1, SPINK1, and CFTR genes
- Autoimmune Pancreatitis
- Recurrent Acute Pancreatitis
- Obstructive Pancreatitis
- Age-related Factors
Symptoms and Signs of Pancreatitis
Symptoms of Acute Pancreatitis:
- Severe Abdominal Pain – In the upper abdomen that may radiate to the back
- Nausea and Vomiting
- Fever
- Yellowing of Skin and Eyes (Jaundice)
- Rapid Heart Rate (Tachycardia)
- Abdominal Swelling and Tenderness
- Difficulty Breathing
Symptoms of Chronic Pancreatitis:
- Persistent Abdominal Pain – Which may worsen after eating
- Vomiting and Nausea
- Weight Loss
- Sever Back Pain
- Unintended Weight Loss
- Fatty Stool (Steatorrhea) – Greasy, foul-smelling stools
- Symptoms of Diabetes – Excessive thirst, frequent urination
- Loss of Appetite
- Fatigue and Weakness
- Digestive Issues and Malabsorption
Lifestyle Challenges for Pancreatitis Patients
Patients with pancreatitis face the following challenges:
- Chronic Pain Management – Managing pain in chronic pancreatitis can be challenging
- Dietary Restrictions – Low-fat diet, small meals, avoiding certain foods
- Alcohol Abstinence – Complete abstinence from alcohol is essential
- Impaired Digestion and Nutrition – Pancreatic enzyme deficiency necessitating enzyme supplements
- Diabetes Management – Chronic pancreatitis often causes diabetes
- Medication Side Effects – From painkillers and other medications
- Frequent Hospitalizations – Due to acute flare-ups
- Mental Health Impact – Depression and anxiety due to chronic pain, dietary restrictions, and reduced quality of life
- Work and Social Life Impact – Work absenteeism and social isolation due to the condition
- Financial Burden – Due to long-term treatment and hospitalizations
Treatment Options for Pancreatitis
Conventional Treatment
For Acute Pancreatitis:
- Hospitalization – Required in most cases
- IV Fluid and Electrolyte Replacement
- Pain Management – Pain-relieving medications
- Food Restriction – To rest the pancreas
- Antibiotics for Infections – If necessary
- Surgical or Endoscopic Intervention – For gallstones or pancreatic necrosis
For Chronic Pancreatitis:
- Pain Management – Pain relievers, sometimes narcotics
- Pancreatic Enzyme Supplements
- Insulin or Oral Hypoglycemic Agents – For diabetes management
- Endoscopic or Surgical Procedures:
- ERCP (Endoscopic Retrograde Cholangiopancreatography)
- Stent Placement
- Pancreatic Drainage Procedures
- Partial or Total Pancreatectomy
Integrated Lifestyle and Natural Treatments
- Dietary Modifications:
- Low-fat diet (<30% of daily calories from fat)
- Small and frequent meals
- Avoiding highly processed foods
- Antioxidant-rich foods (fruits and vegetables)
- Adequate protein and carbohydrates
- Alcohol and Smoking Cessation:
- Complete abstinence from alcohol
- Quitting smoking
- Hydration:
- Drinking adequate water daily (approximately 2-3 liters)
- Ayurvedic Treatments:
- Triphala Churna
- Shatavari
- Ashwagandha
- Giloy
- Yoga and Pranayama:
- Vajrasana
- Pawanmuktasana
- Ardha Matsyendrasana
- Anulom-Vilom Pranayama
- Bhramari Pranayama
- Herbs and Supplements:
- Curcumin (Turmeric)
- Omega-3 Fatty Acids
- Probiotics
- Vitamin D and Calcium
- Stress Management:
- Meditation
- Deep Breathing Exercises
- Mind-Body Techniques
Conventional vs. Integrated Treatment: Comparative Chart
| Aspect | Conventional Treatment | Integrated Lifestyle Treatment |
|---|---|---|
| Approach | Symptom-focused | Holistic approach |
| Focus | Immediate relief and complication management | Addressing root causes and promoting wellness |
| Effectiveness | Faster relief in acute phase | Better in long-term management |
| Side Effects | More likely (especially from pain medications) | Lower risk |
| Cost | Generally more expensive | More economical in the long run |
| Patient Participation | Less required | Highly required |
| Recurrence Prevention | Limited | Better outcomes |
| Quality of Life | May be reduced during treatment | Likely to improve |
What is Pancreatitis – Effective Management
Long-term Management Strategies:
Regular Medical Check-ups:
- Evaluation of pancreatic function
- Monitoring for diabetes
- Assessment of nutritional status
Self-care:
- Symptom monitoring
- Recognising warning signs
- Medication adherence
- Following dietary guidelines
Support Groups:
- Sharing experiences
- Gaining emotional support
- Obtaining practical advice
Integrated Approach:
- Conventional medicine
- Ayurveda
- Lifestyle modifications
- Dietary therapy
Living a Long and Healthy Life with Pancreatitis
Essential steps for living a healthy and meaningful life with pancreatitis:
- Complete Abstinence from Alcohol – This is the most crucial step
- Adopting Healthy Dietary Patterns – Low fat, high fiber
- Quitting Smoking
- Regular Physical Activity – Light to moderate exercise
- Maintaining Adequate Hydration
- Following Medical Instructions – Medications and supplements
- Adopting Stress Management Techniques
- Building a Support Network – Family, friends, and support groups
- Regular Medical Check-ups – Monitoring pancreatic condition
- Positive Mental Attitude – Learning to live with the condition
Conclusion
Pancreatitis is a serious condition that requires proper management. While it can be challenging, with a combination of healthy lifestyle choices, dietary modifications, and appropriate medical care, patients can control their symptoms and lead a healthy life.
If you or your loved one is struggling with pancreatitis, book an appointment with our specialists today. Our integrated approach can help you effectively manage your condition and achieve a better quality of life.
Take the Next Step Toward Healing
Who is Mr. Vivek Singh Sengar?
Mr. Vivek Singh Sengar is an experienced Clinical Nutritionist and the Founder of Fit My Heart. With over 11 years of experience, he has helped thousands of patients reverse liver, pancreas, heart, and metabolic diseases through non-invasive and drug-free methods. His mission is to provide root-cause healing through lifestyle and nutrition.
📲 Book Your Consultation Now
If you or someone in your family is suffering from Pancreatitis, don’t delay.
👉 Consult us today and take your first step toward a pain-free, healthy life.
Frequently Asked Questions About Pancreatitis
Understanding Pancreatitis
1. What is pancreatitis?
Pancreatitis is inflammation of the pancreas, a gland located behind the stomach that produces digestive enzymes and insulin. The inflammation occurs when digestive enzymes become activated while still in the pancreas, causing irritation and damage to the organ’s tissues.
2. What is the difference between acute and chronic pancreatitis?
Acute pancreatitis is sudden inflammation that typically resolves within days to weeks with proper treatment. Chronic pancreatitis is persistent inflammation that develops over many years, causing permanent damage to the pancreas and impairing its function.
3. What are the main causes of pancreatitis?
The most common causes of acute pancreatitis are gallstones (40-50% of cases) and excessive alcohol consumption (30-35% of cases). Chronic pancreatitis is primarily caused by long-term alcohol abuse (70% of cases), genetic factors, recurrent acute pancreatitis, and autoimmune conditions.
Symptoms and Diagnosis
4. What are the warning signs of pancreatitis?
The primary symptom is severe upper abdominal pain that may radiate to the back. Other symptoms include nausea, vomiting, fever, rapid heart rate, and tender abdomen. Chronic pancreatitis may additionally present with weight loss, oily stools, and symptoms of diabetes.
5. When should I seek emergency medical attention for suspected pancreatitis?
Seek immediate medical care if you experience severe abdominal pain (especially with nausea and vomiting), pain so intense you cannot find a comfortable position, abdominal pain radiating to your back, fever with abdominal pain, or yellowing of the skin or eyes.
6. How is pancreatitis diagnosed?
Diagnosis typically involves blood tests to measure pancreatic enzyme levels (amylase and lipase), imaging studies such as CT scans or ultrasound, and sometimes more specialized tests like endoscopic ultrasound or ERCP (Endoscopic Retrograde Cholangiopancreatography).
Treatment and Management
7. Can pancreatitis be cured?
Acute pancreatitis can often be resolved with proper treatment. Chronic pancreatitis, however, cannot be cured as the damage is permanent, but symptoms can be managed effectively with appropriate treatment and lifestyle modifications.
8. What dietary changes are recommended for pancreatitis patients?
Patients should follow a low-fat diet (less than 30% of daily calories from fat), eat smaller and more frequent meals, avoid alcohol completely, limit processed foods, increase consumption of fruits and vegetables, and stay well-hydrated.
9. Why is alcohol abstinence so important for pancreatitis patients?
Alcohol directly damages pancreatic cells and is a major cause of both acute and chronic pancreatitis. Even small amounts can trigger severe pain and inflammation in patients with existing pancreatic damage. Complete abstinence is essential to prevent further damage and recurrent attacks.
10. What medications are used to treat pancreatitis?
Treatments may include pain medications, pancreatic enzyme supplements (for chronic pancreatitis), insulin (if diabetes develops), and sometimes antibiotics (if infection is present). The specific medications depend on the type of pancreatitis and individual symptoms.
Complications and Long-term Outlook
11. What are the potential complications of untreated pancreatitis?
Untreated pancreatitis can lead to serious complications including pancreatic necrosis (tissue death), pseudocysts, infection, kidney failure, breathing problems, diabetes, malnutrition, and in severe cases, multi-organ failure or death.
12. Does pancreatitis increase the risk of pancreatic cancer?
Yes, chronic pancreatitis is associated with an increased risk of pancreatic cancer. The risk is approximately 5% within 20 years of diagnosis and is higher in those with hereditary forms of pancreatitis.
Natural Approaches and Prevention
13. Can yoga and meditation help manage pancreatitis?
Yes, certain yoga postures like Vajrasana, Pawanmuktasana, and Ardha Matsyendrasana may help improve digestion and reduce stress. Breathing exercises (pranayama) and meditation can help manage pain and reduce stress, which may help prevent flare-ups.
14. What supplements may be beneficial for pancreatitis patients?
Some potentially beneficial supplements include curcumin (from turmeric) for its anti-inflammatory properties, omega-3 fatty acids to reduce inflammation, probiotics to support gut health, and vitamin D and calcium supplements to prevent osteoporosis, which is common in chronic pancreatitis.
15. How can I prevent pancreatitis recurrence?
Prevention strategies include complete abstinence from alcohol, following a low-fat diet, quitting smoking, maintaining a healthy weight, staying hydrated, taking prescribed medications as directed, attending regular medical check-ups, and promptly treating any underlying conditions like gallstones or high triglycerides.
EECP Therapy for Heart Failure: A Revolutionary Non-Invasive Treatment Option
Posted byEECP Therapy for Heart Failure: Heart failure affects millions worldwide, causing significant suffering and economic burden. Among the various treatment options available today, Enhanced External Counterpulsation (EECP) therapy for heart failure has emerged as a promising non-invasive approach, particularly for patients with ischemic heart failure. This blog explores the science behind EECP therapy for heart failure, its effectiveness, ideal candidates, and what patients can expect from this treatment.
Understanding Heart Failure
Heart failure occurs when the heart cannot pump enough blood to meet the body’s needs. Despite its name, heart failure doesn’t mean the heart has stopped working—rather, it means the heart isn’t working as efficiently as it should. This serious condition affects approximately 6.2 million adults in the United States alone.
Types of Heart Failure
Heart failure can be categorized based on which side of the heart is affected:
Left-sided heart failure: The most common type, occurs when the left ventricle cannot pump blood effectively
Right-sided heart failure: Often results from left-sided failure, occurs when the right ventricle cannot effectively pump blood to the lungs
Biventricular heart failure: Affects both sides of the heart
Heart failure can also be classified based on ejection fraction (EF)—the percentage of blood pumped out with each contraction:
Heart failure with reduced ejection fraction (HFrEF): EF less than 40%
Heart failure with preserved ejection fraction (HFpEF): EF greater than or equal to 50%
Heart failure with mid-range ejection fraction: EF between 40-49%
Causes of Heart Failure
The primary causes of heart failure include:
- Coronary artery disease (CAD): According to research, CAD is responsible for approximately 48.3% of heart failure cases in China and remains a leading cause worldwide
- Hypertension
- Valvular heart disease
- Cardiomyopathy
- Congenital heart defects
- Arrhythmias
- Diabetes
- Alcohol or drug abuse
Symptoms of Heart Failure
Common symptoms include:
- Shortness of breath during activity or when lying down
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Reduced ability to exercise
- Persistent cough or wheezing
- Increased need to urinate, especially at night
- Sudden weight gain from fluid retention
Conventional Treatments for Heart Failure
Before diving into EECP therapy for heart failure, let’s review the conventional treatment approaches:
Medications
Standard medications for heart failure include:
- ACE inhibitors or ARBs to widen blood vessels
- Beta-blockers to slow heart rate and reduce blood pressure
- Diuretics to reduce fluid buildup
- Aldosterone antagonists to help the body eliminate salt and water
- SGLT2 inhibitors, which have shown remarkable benefits in recent years
- Angiotensin receptor-neprilysin inhibitors (ARNIs)
- Digoxin to strengthen heart contractions
- Anticoagulants to prevent blood clots
Devices and Surgical Interventions
When medications aren’t enough, doctors may recommend:
- Implantable cardioverter-defibrillators (ICDs)
- Cardiac resynchronization therapy (CRT)
- Left ventricular assist devices (LVADs)
- Heart valve repair or replacement
- Coronary bypass surgery
- Heart transplantation
Despite these options, many patients continue to experience symptoms or may not be eligible for invasive procedures. This is where EECP therapy for heart failure comes into the picture.
What is EECP Therapy for Heart Failure?
Enhanced External Counterpulsation (EECP) is a non-invasive treatment that uses carefully timed compression of the lower extremities to increase blood flow to the heart. The therapy involves wrapping pressure cuffs around the patient’s calves, thighs, and buttocks. These cuffs inflate and deflate in sync with the patient’s heartbeat:
- During diastole (when the heart is relaxing): The cuffs inflate sequentially from the calves upward
- During systole (when the heart is contracting): The cuffs rapidly deflate
This sequential compression creates a “counterpulsation” effect that:
- Increases blood flow to the coronary arteries during diastole
- Decreases cardiac afterload during systole
- Enhances venous return to the heart
A standard course of EECP therapy for heart failure typically consists of 35 one-hour sessions, usually administered 5 days a week for 7 weeks.
The Potential Mechanisms by Which EECP Improves Heart Function:
At this stage, the effects of EECP are primarily categorized into immediate hemodynamic changes and long-term anti-ischemic benefits driven by shear stress, though other potential mechanisms remain to be explored.
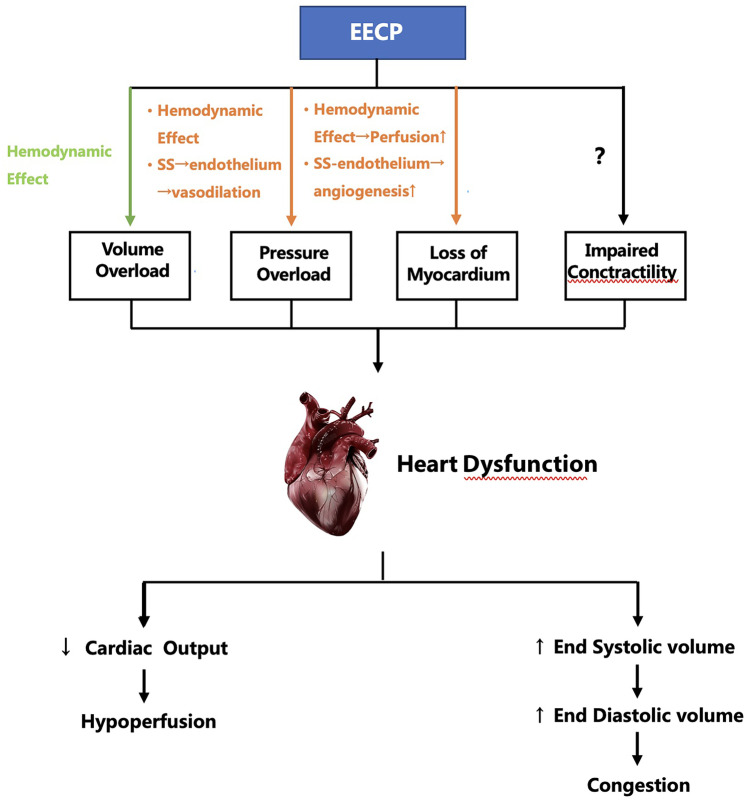
The potential mechanisms by which EECP improves heart failure. EECP, enhanced external counterpulsation; SS, shear stress; green arrow: may be harmful; orange arrow: helpful
EECP Therapy for Heart Failure: The Science of Working
The research paper provides valuable insights into the mechanisms by which EECP therapy improves heart failure:
Immediate Hemodynamic Effects
- Increased coronary perfusion: EECP therapy increases diastolic blood pressure by 26-157%, significantly improving blood flow to the heart muscle
- Reduced cardiac afterload: Synchronous release of all cuffs during systole can reduce systolic blood pressure by 9-16 mmHg
- Decreased left ventricular energy consumption: Studies using pulse wave analysis technology found reduced myocardial oxygen demand after EECP treatment
Long-term Effects Mediated by Shear Stress
EECP therapy for heart failure creates beneficial shear stress on blood vessel walls, which leads to:
Improved endothelial function:
- Increased production of nitric oxide (NO) and other vasodilators
- Decreased production of endothelin-1 (ET-1) and other vasoconstrictors
- Enhanced endothelial cell-dependent vasodilation
Angiogenesis (formation of new blood vessels):
- Upregulation of vascular endothelial growth factor (VEGF)
- Increased angiopoietin production
- Enhanced proliferation and differentiation of endothelial progenitor cells
Anti-inflammatory and anti-atherosclerotic effects:
- Regulation of inflammatory factors
- Reduction in oxidative stress
- Stabilization of atherosclerotic plaques
Potential direct effects on cardiac contractility:
- Increased plasma adrenomedullin (ADM) levels
- Possible improvements in mitochondrial function
- Potential effects on calcium ion currents in ventricular myocytes
These mechanisms collectively contribute to improved myocardial perfusion, reduced cardiac workload, and enhanced heart function.
Clinical Evidence for EECP Therapy in Heart Failure
Multiple studies have demonstrated the benefits of EECP therapy for heart failure patients:
The PEECH Study
This randomized controlled trial included 130 patients with ischemic heart failure (NYHA class II-III) and found:
- Significant improvements in NYHA classification
- Enhanced quality of life
- Increased total exercise time
- Higher peak oxygen uptake (VO₂peak) one week after treatment
Effects on Performance Status
Studies consistently show that EECP therapy for heart failure improves:
- Exercise capacity (total exercise time)
- 6-minute walk test performance
- NYHA functional classification
Effects on Cardiac Function
Systolic Function
Results on left ventricular ejection fraction (LVEF) are mixed:
- Some studies show no significant improvement
- Others demonstrate marked improvement, especially in patients with baseline LVEF <40%
- Global longitudinal strain (GLS) measurements show promising improvements
Diastolic Function
Studies consistently show improvements in diastolic function markers:
- Enhanced E/A ratio (0.92 ± 0.41 vs. 1.08 ± 0.46, P<0.05)
- Improved E/Ea ratio (12.61 ± 4.22 vs. 15.44 ± 6.96, P<0.05)
- Better peak filling rate (PFR)
The E/A ratio is a measurement used to assess cardiac diastolic function (how well the heart fills with blood between contractions), which I mentioned in the “Effects on Cardiac Function” section of the blog post.
The E/A ratio is an echocardiographic measurement derived from Doppler imaging that evaluates how blood flows through the mitral valve between the left atrium and left ventricle during diastole (the filling phase of the cardiac cycle). It consists of two components:
- E wave (Early diastolic filling): Represents passive filling of the ventricle when the mitral valve first opens. This is the first and usually larger peak on the Doppler waveform.
- A wave (Atrial contraction): Represents the additional blood flow into the ventricle caused by atrial contraction (the “atrial kick”). This is the second peak on the Doppler waveform.
The E/A ratio is calculated by dividing the peak E wave velocity by the peak A wave velocity.
From the Research it has been found that, patients who received EECP therapy showed an improvement in their E/A ratio from 0.92 ± 0.41 to 1.08 ± 0.46 (P < 0.05), indicating enhanced diastolic function after treatment.
A normal E/A ratio typically ranges from about 0.8 to 2.0, depending on age. In heart failure with diastolic dysfunction, this ratio is often abnormal:
- In early/mild diastolic dysfunction: The ratio may be reduced (<0.8)
- In moderate diastolic dysfunction: The ratio may appear pseudonormal (normal-looking but with other abnormal parameters)
- In severe diastolic dysfunction: The ratio may be elevated (>2.0), known as a “restrictive filling pattern”
The improvement in E/A ratio after EECP therapy suggests that this treatment helps the heart fill more efficiently during diastole, which is particularly important for heart failure patients.
Effects on Prognosis
EECP therapy for heart failure appears to improve short-term outcomes:
- Reduced 90-day readmission rates (6.1% vs. predicted 34%)
- 78% reduction in emergency room visits over 6 months
- 73% reduction in hospitalizations over 6 months
Ideal Candidates for EECP Therapy for Heart Failure
Based on clinical studies and guidelines, the following patients may benefit most from EECP therapy:
Recommended Candidates:
- Patients with stable ischemic heart failure (NYHA class II-III)
- Individuals with angina symptoms combined with heart failure
- Heart failure patients with coronary artery disease as the primary cause
- Patients who have exhausted standard medical therapies
- Individuals who are not candidates for invasive procedures
- Elderly patients (studies show particularly good results in those over 65)
- Patients seeking to improve exercise tolerance and quality of life
Comparing EECP Therapy with Surgical Options and ICDs
When considering treatments to improve heart function, patients and clinicians have several options. Here’s how EECP therapy for heart failure compares to surgical interventions and implantable devices:
| Aspect | EECP Therapy for Heart Failure | Heart Surgery (CABG/Valve) | ICD/CRT Devices |
|---|---|---|---|
| Invasiveness | Non-invasive, external | Highly invasive | Minimally invasive |
| Anesthesia | None required | General anesthesia | Local anesthesia |
| Hospital stay | Outpatient procedure | 5-7 days | 1-2 days |
| Recovery time | None, resume normal activities | 6-12 weeks | 1-2 weeks |
| Treatment duration | 35 one-hour sessions over 7 weeks | One-time procedure | One-time implantation |
| Mechanism | Increases coronary perfusion, reduces afterload | Direct revascularization or valve repair | Corrects rhythm or synchronizes contractions |
| Effect on survival | Limited data on long-term survival | Improved survival in selected patients | Improved survival in appropriate candidates |
| Effect on symptoms | Significant symptom improvement | Variable symptom improvement | Variable symptom improvement |
| Exercise capacity | Consistently improved | Variable improvement | Variable improvement |
| Risk of serious complications | Very low | Moderate to high | Low to moderate |
| Retreatment possibility | Can be repeated as needed | Redo surgery is high risk | Battery replacement needed every 5-10 years |
| Cost | Moderate | Very high | High |
| Insurance coverage | Variable | Generally covered | Generally covered |
Contraindications: Who Should Not Receive EECP Therapy for Heart Failure
Although EECP therapy for heart failure is generally safe, it’s not appropriate for everyone. Contraindications include:
Absolute Contraindications:
- Acute heart failure decompensation
- Severe aortic insufficiency (regurgitation)
- Acute deep vein thrombosis (DVT)
- Severe peripheral arterial disease with ulcers
- Pregnancy
- Arrhythmias that interfere with ECG triggering
- Coagulopathy with active bleeding
Relative Contraindications:
- Hypertension uncontrolled by medication (>180/110 mmHg)
- Recent cardiac catheterization or arterial puncture (<2 weeks)
- Severe chronic obstructive pulmonary disease
- Abdominal aortic aneurysm >4 cm
- Moderate to severe aortic stenosis
- Recent stroke (<3 months)
- Heart rate >120 beats per minute
What to Expect During EECP Therapy for Heart Failure
For patients considering EECP therapy, here’s a guide to the treatment experience:
Before Treatment:
- Comprehensive evaluation: Medical history review, physical examination, and possibly cardiac tests
- Treatment planning: Discussion of the number of sessions needed (typically 35)
- Insurance verification: Checking coverage for the procedure
During Treatment:
Preparation:
- The patient lies on a comfortable treatment table
- ECG electrodes are attached to monitor heart rhythm
- Blood pressure cuff is placed on one arm
- Pressure cuffs are wrapped around calves, thighs, and buttocks
The procedure:
- Each session lasts approximately one hour
- The cuffs inflate and deflate in sync with the heartbeat
- Patients may feel pressure similar to a tight hug on their legs
- Most patients find the treatment comfortable enough to read, watch TV, or even nap
Monitoring:
- Heart rhythm and blood pressure are continuously monitored
- Healthcare providers check for any discomfort or side effects
After Treatment:
Immediate effects:
- Most patients can resume normal activities immediately
- Some may experience mild fatigue or muscle soreness
Follow-up care:
- Regular assessments throughout the course of therapy
- Evaluation of symptoms and functional capacity
- Adjustment of medications as needed
Potential side effects:
- Minor discomfort like skin irritation or bruising
- Muscle or joint soreness
- Rarely, dizziness or fatigue
Expected Outcomes:
Based on clinical studies, patients may experience:
- Noticeable improvement in symptoms after 15-20 sessions
- Reduced shortness of breath
- Increased exercise tolerance
- Better quality of life
- Decreased need for nitrate medications (if used for angina)
- Reduction in emergency room visits and hospitalizations
The Future of EECP Therapy for Heart Failure
As research continues, several exciting developments are on the horizon:
- Personalized treatment protocols: Tailoring the number and frequency of sessions to individual patient needs
- Combination therapies: Integrating EECP with other treatments for synergistic effects
- Improved devices: More comfortable, efficient, and portable EECP machines
- Expanded indications: Potential use in other cardiovascular conditions
- Long-term efficacy data: More research on the durability of benefits
Conclusion
EECP therapy for heart failure represents a valuable non-invasive option for patients with ischemic heart failure, particularly those who have exhausted conventional treatments or are not candidates for invasive procedures. The therapy’s ability to improve myocardial perfusion, reduce cardiac workload, and enhance both systolic and diastolic function makes it a promising addition to the heart failure treatment arsenal.
Clinical evidence demonstrates that EECP therapy for heart failure can significantly improve functional capacity, quality of life, and short-term outcomes like hospitalizations. While more research is needed—especially regarding long-term benefits and direct effects on cardiac contractility—the existing data supports EECP therapy for heart failure as a safe and effective treatment option.
For heart failure patients seeking symptom relief and improved quality of life, EECP therapy for heart failure deserves consideration as part of a comprehensive treatment plan. As with any medical treatment, patients should consult with their cardiologists to determine if EECP therapy for heart failure is appropriate for their specific condition.
Meet Vivek Singh Sengar – EECP Expert & Founder of Fit My Heart
Vivek Singh Sengar is a renowned Clinical Nutritionist and EECP Therapy Specialist, with over 11 years of experience in reversing heart failure and coronary blockages through non-invasive, drug-free treatments. As the Founder of Fit My Heart, he has helped thousands of patients avoid bypass surgery and improve their heart function using personalized EECP therapy and lifestyle protocols.
✅ Struggling with Heart Failure?
You Deserve a Second Opinion – Without Surgery or Stents
🔹 Book a FREE 15-minute consultation with Vivek Singh Sengar
🔹 Understand if EECP Therapy is right for your heart condition
🔹 Get a personalized, non-surgical treatment plan
👉 Book Your Free Consultation Now
Take the first step toward a stronger heart – naturally.
Frequently Asked Questions About EECP Therapy for Heart Failure
Que: What exactly is EECP therapy for heart failure?
Ans: EECP is a non-invasive treatment that uses inflatable cuffs on the legs to increase blood flow to the heart and improve cardiac function by synchronizing compression with the patient’s heartbeat.
Que: How long does a complete course of EECP therapy take?
Ans: A standard course consists of 35 one-hour sessions, typically administered 5 days a week for 7 weeks.
Que: Is EECP therapy painful?
Ans: No, it’s not painful. Most patients describe a sensation of pressure similar to a tight hug on their legs, and many find it comfortable enough to read or nap during treatment.
Que: How soon might I notice improvements with EECP therapy for heart failure?
Ans: Many patients report noticeable symptom improvement after 15-20 sessions, though individual responses vary.
Que: Is EECP therapy covered by insurance?
Ans: In USA Coverage varies by provider. EECP is covered by Medicare and many insurance plans for specific indications, but verification is recommended before starting treatment. In INDIA, insurance companies usually do not cover EECP Treatment, but It purely depends upon the patient and doctor. Usually, a patient is required to talk to his doctor and insurance company. It has been seen that many patients get the reimbursement after submitting all the valid documents and consistent follow-up with the insurance company and the doctor.
Que: Can EECP therapy replace medications for heart failure?
Ans: No, EECP is typically used as a complementary treatment alongside standard medications, not as a replacement but in most of the cases the need for medicines is reduced post EECP therapy.
Que: Are the effects of EECP therapy permanent?
Ans: Benefits typically last 3-5 years, after which some patients may require repeat courses of therapy or booster doze can be taken to maintain the effect of EECP Therapy.
Que: Can I have EECP therapy if I have an ICD or pacemaker?
Ans: Yes, having a pacemaker or ICD is not a contraindication for EECP therapy.
Que: What side effects might occur with EECP therapy?
Ans: Common side effects are mild and include skin irritation, muscle soreness, or fatigue. Serious side effects are rare.
Que: How does EECP therapy differ from cardiac rehabilitation?
Ans: While cardiac rehab focuses on exercise and lifestyle changes, EECP is a passive treatment that mechanically improves blood flow without requiring physical exertion.
Que: Can EECP therapy help if I’m waiting for a heart transplant?
Ans: Yes, EECP may be used as a “bridge therapy” to improve quality of life and function while waiting for transplantation, in most cases EECP Therapy may avoid the need for the Heart Transplantation.
Que: Is there an age limit for EECP therapy?
Ans: There’s no specific age limit, and studies show elderly patients (over 65) often respond particularly well to treatment.
Que: Can EECP therapy reduce my need for heart medications?
Ans: Most of the patients require fewer medications after EECP therapy, but any changes should only be made under physician supervision.
Que: How is success of EECP therapy measured?
Ans: Success is measured through improved symptoms, exercise capacity, quality of life, echocardiographic parameters, and reduced hospitalizations.
Que: Can I resume normal activities while undergoing EECP therapy?
Ans: Yes, most patients can maintain their normal daily activities during the treatment period with no restrictions.
What is EECP Treatment: Best Non – Surgical Alternative of Angioplasty and Bypass Surgery
Posted byThe EECP treatment system consists of three main components:
- Adjustable cuffs that wrap around the patient’s calves, thighs, and buttocks
- An electrocardiogram (ECG) to monitor heart rhythm
- A computerized control system that synchronizes cuff inflation and deflation with the patient’s cardiac cycle
How does EECP therapy work?
The mechanism behind EECP treatment involves carefully timed counterpulsation that works in harmony with the heart’s natural rhythm. During EECP treatment:
- Diastole Phase: When the heart is at rest (diastole), the cuffs rapidly inflate sequentially from the calves upward, creating a wave-like compression that propels blood back toward the heart. This retrograde pressure during EECP treatment increases coronary perfusion pressure and blood flow to the myocardium.
- Systole Phase: Just before the heart contracts (systole), the cuffs rapidly deflate simultaneously, reducing the resistance the heart must pump against. This “systolic unloading” during EECP treatment decreases the heart’s workload and oxygen demand.
This precisely timed sequence in EECP treatment creates several beneficial hemodynamic effects:
- Increased coronary blood flow
- Enhanced venous return to the heart
- Reduced cardiac workload
- Improved oxygen supply to the heart muscle
Mechanism of Action
EECP treatment works through multiple physiological pathways that collectively improve cardiovascular function:
Hemodynamic Effects of EECP Treatment
The immediate hemodynamic benefits of EECP treatment include:
- Increased diastolic pressure, improving coronary perfusion by 20-40%
- Decreased systolic pressure, reducing cardiac afterload
- Improved cardiac output and stroke volume
- Enhanced venous return
Vascular Effects during EECP Treatment
EECP treatment generates significant changes in the vascular system:
Development of New Blood Vessels
EECP treatment stimulates angiogenesis (formation of new blood vessels) through:
- Increased shear stress on vessel walls
- Upregulation of vascular endothelial growth factor (VEGF)
- Activation of the hypoxia-inducible factor 1-alpha (HIF-1α) pathway
- Release of stem cell mobilizing factors
These processes during EECP treatment lead to the formation of new capillary networks that improve blood flow to oxygen-deprived tissues.
Dilation of Existing Blood Vessels
EECP treatment enhances vasodilation through:
- Increased nitric oxide (NO) production
- Improved endothelial function
- Reduced endothelin-1 levels (a potent vasoconstrictor)
- Decreased sympathetic nervous system activity
Cellular and Molecular Mechanisms
At the cellular level, EECP treatment triggers:
- Increased production of endothelial progenitor cells
- Reduced inflammation markers (C-reactive protein, tumor necrosis factor-alpha)
- Improved peripheral vascular resistance
- Enhanced oxygen utilization at the tissue level
What conditions can EECP therapy treat?
EECP treatment has been approved for and shown efficacy in treating numerous cardiovascular and related conditions:
Primary Applications of EECP Treatment
- Chest pain (Angina): EECP treatment is FDA-approved for chronic, stable angina that doesn’t respond adequately to medication or isn’t suitable for invasive procedures.
- Coronary artery disease: EECP treatment improves blood flow in patients with significant coronary blockages.
- Shortness of breath (dyspnea): Many patients report improved breathing capacity after EECP treatment.
- Fatigue: EECP treatment can increase energy levels by improving overall circulatory function.
- Cough: Some patients with cardiac-related cough experience symptom relief after EECP treatment.
Other Conditions Benefiting from EECP Treatment
EECP treatment has shown promising results for:
- Cardiac syndrome X: EECP treatment improves microvascular function in patients with angina but normal coronary arteries.
- Heart failure: EECP treatment enhances cardiac function and exercise capacity in heart failure patients.
- Left ventricular dysfunction: EECP treatment can improve ejection fraction and cardiac performance.
- Cerebrovascular disease: EECP treatment may enhance cerebral circulation and cognitive function.
- Kidney (renal) failure: EECP treatment can improve renal perfusion and potentially slow disease progression.
- Peripheral artery disease (PAD): EECP treatment increases collateral circulation in the extremities.
- Erectile dysfunction: By improving vascular function, EECP treatment may benefit men with vascular-related erectile dysfunction.
- Lung disease: Some patients with pulmonary hypertension show improvement with EECP treatment.
- Diabetes: EECP treatment may improve peripheral circulation and reduce diabetes-related complications.
Who is eligible for EECP therapy?
Ideal candidates for EECP treatment include:
- Patients with chronic, stable angina who have exhausted medication options
- Individuals who are not candidates for bypass surgery or angioplasty
- Patients seeking non-invasive alternatives to surgical interventions
- Those with persistent symptoms despite prior revascularisation procedures
- Patients with multiple risk factors who want to improve their cardiovascular health
Before starting EECP treatment, patients undergo a comprehensive evaluation including:
- Complete medical history
- Physical examination
- Cardiovascular assessments
- Evaluation of symptom severity and frequency
Who Should Not Undergo EECP Treatment?
EECP treatment is contraindicated or requires special consideration in patients with:
- Severe Aortic insufficiency: The increased diastolic pressure from EECP treatment may worsen this condition.
- Atrial fibrillation (Afib): Irregular heartbeats can interfere with proper EECP treatment timing.
- Blood clots: EECP treatment may dislodge existing clots.
- Congenital heart disease: Certain structural abnormalities may complicate EECP treatment.
- Sever Enlarged heart (cardiomegaly): May affect EECP treatment effectiveness.
- Heart valve disease: Especially severe mitral or aortic regurgitation.
- Hemorrhage: Active bleeding is a contraindication for EECP treatment.
- Severe hypertension: Uncontrolled high blood pressure must be managed before EECP treatment.
- Irregular heartbeat or fast heart rate (tachycardia): These can interfere with EECP treatment synchronization.
- Hypertrophic cardiomyopathy: The altered hemodynamics may be problematic.
- Pulmonary hypertension (PH): Severe cases require careful evaluation before EECP treatment.
- Severe peripheral vascular disease: May limit the effectiveness of EECP treatment.
- Recent cardiac catheterization: Typically requires a waiting period before EECP treatment.
- Pregnancy: EECP treatment has not been studied in pregnant women.
- Deep vein thrombosis: Increases risk of complications during EECP treatment.
Is EECP therapy a common procedure?
While EECP treatment has been FDA-approved since 1995 and has gained recognition worldwide, it isn’t as widely available as some conventional cardiac procedures. The popularity of EECP treatment varies by region:
- In the United States, over 1,200 centers offer EECP treatment
- EECP treatment has received approval from regulatory bodies in Europe, Asia, and Australia
- The International EECP Patient Registry has documented outcomes for over 30,000 patients who have undergone EECP treatment
- More than 20,000 EECP treatment procedures are performed annually in the US alone
Despite its proven benefits, EECP treatment remains underutilized partly due to:
- Limited awareness among both patients and healthcare providers
- Insurance coverage variations
- The substantial time commitment required for the full EECP treatment course
International Approvals for EECP Treatment
EECP treatment has received regulatory approval from numerous health authorities worldwide:
- FDA approval in the United States (1995)
- CE Mark in Europe
- PMDA approval in Japan
- TGA approval in Australia
- CDSCO approval in India
- NMPA (formerly CFDA) approval in China
These approvals reflect the growing body of evidence supporting EECP treatment’s safety and efficacy, with international clinical guidelines increasingly recognizing EECP treatment as an important therapeutic option for selected patients.
The EECP Treatment Experience
What happens before EECP therapy?
Preparation for EECP treatment involves:
- Initial consultation: A specialist evaluates the patient’s medical history, current symptoms, and treatment goals for EECP treatment.
- Baseline assessments: Before starting EECP treatment, measurements typically include:
- Blood pressure and heart rate
- Electrocardiogram (ECG)
- Exercise capacity evaluation
- Quality of life questionnaires
- Blood tests to assess cardiac biomarkers
- Education: Patients receive detailed information about the EECP treatment process, expected outcomes, and timeline.
- Clothing guidance: Patients are advised to wear comfortable, loose-fitting clothing to EECP treatment sessions.
What happens during EECP therapy?
A typical EECP treatment session follows this sequence:
- The patient lies comfortably on a treatment table.
- Three sets of pressure cuffs are wrapped around the calves, lower thighs, and upper thighs/buttocks.
- ECG electrodes are placed to monitor heart rhythm and synchronize the EECP treatment system.
- A finger plethysmograph monitors blood pressure waves during EECP treatment.
- The computer-controlled system inflates and deflates the cuffs in precise timing with the cardiac cycle.
- During EECP treatment, patients can read, watch television, or even nap.
- Medical staff regularly check the patient’s comfort and vital signs throughout the EECP treatment session.
Many patients report that EECP treatment feels like a strong massage of the legs and buttocks, with a squeezing sensation moving up the legs during each heartbeat.
How long does EECP therapy last?
The standard EECP treatment protocol consists of:
- 35 one-hour sessions
- Usually scheduled 5 days per week
- The full course typically takes 7 weeks to complete
- Each EECP treatment session includes a few minutes for setup and removal of the cuffs
Some variations in EECP treatment scheduling may occur based on individual needs:
- Extended protocols (up to 50 sessions) for severe conditions
- Compressed schedules (twice daily sessions) for patients traveling from distant locations
- Maintenance EECP treatment sessions (monthly or quarterly) for some patients after completing the initial course
The commitment to a full EECP treatment course is crucial for optimal results, as the beneficial effects of EECP treatment are cumulative.
Read Also: EECP Treatment for Chest Pain
Recovery and Outlook
Patient Experience after EECP therapy
Patient experiences during and after EECP treatment vary:
- During early sessions: Some patients may experience fatigue after EECP treatment as their body adjusts to the therapy.
- Mid-course: Many begin noticing improvements in symptoms by the 15-20th EECP treatment session.
- Upon completion: Most patients report significant improvement in:
- Exercise capacity
- Reduction in angina episodes
- Decreased need for nitroglycerin
- Improved quality of life
- Enhanced energy levels
Recovery time from EECP
One of the significant advantages of EECP treatment is the minimal recovery time:
- No downtime between sessions
- Patients can return to normal activities immediately after each EECP treatment
- No hospitalization required
- No wound care or activity restrictions
- Patients can drive themselves to and from EECP treatment appointments
This makes EECP treatment particularly suitable for:
- Elderly patients
- Those with multiple comorbidities
- Individuals who cannot afford extended time away from work or family responsibilities
Can I have EECP therapy more than once?
Many patients benefit from repeat courses of EECP treatment:
- Initial benefits of EECP treatment typically last 3-5 years for most patients
- When symptoms begin to return, a repeat course of EECP treatment is often beneficial
- Some patients receive a “booster” course of 15-20 EECP treatment sessions at regular intervals
- Maintenance protocols may involve periodic single EECP treatment sessions to sustain benefits
There is no limit to the number of EECP treatment courses a patient can receive over their lifetime, provided they remain appropriate candidates.
Risks and Benefits
What are the advantages of EECP therapy?
EECP treatment offers numerous benefits:
- Non-invasive: EECP treatment requires no incisions, anesthesia, or radiation exposure.
- Outpatient procedure: EECP treatment requires no hospitalization.
- Cumulative benefits: The effects of EECP treatment continue to improve over the course of therapy.
- Sustained results: Benefits often last 3-5 years after a course of EECP treatment.
- Improved exercise capacity: Most patients show significant functional improvement after EECP treatment.
- Reduced medication needs: Many patients require fewer anti-anginal medications after EECP treatment.
- Fewer angina episodes: The frequency and intensity of chest pain typically decrease with EECP treatment.
- Enhanced quality of life: Patients report better daily functioning after EECP treatment.
- Safe for multiple courses: EECP treatment can be repeated when symptoms return.
- Complementary therapy: EECP treatment works well alongside conventional treatments.
What are the risks or complications of EECP therapy?
EECP treatment is generally very safe, with minimal risks:
- Skin irritation or bruising: The most common side effect of EECP treatment, occurring in about 5-10% of patients.
- Edema: Mild swelling in the legs may occur during the EECP treatment course but typically resolves quickly.
- Fatigue: Some patients experience temporary tiredness after initial EECP treatment sessions.
- Muscle or joint discomfort: Minor aches may occur as the body adjusts to EECP treatment.
- Numbness or tingling: Occasionally reported during EECP treatment sessions but resolves when pressure is released.
- Pressure sores: Rare with modern EECP treatment equipment and proper technique.
Serious complications from EECP treatment are extremely rare, with studies reporting rates below 0.5%.
Conclusion
EECP treatment represents a significant advancement in non-invasive cardiovascular therapy, offering hope to patients who have limited options or have not responded adequately to conventional treatments. This FDA-approved therapy leverages the body’s natural circulatory mechanics to improve blood flow, stimulate new vessel formation, and enhance overall cardiovascular function.
For patients with angina, heart failure, and various other cardiovascular conditions, EECP treatment provides a safe, effective option with minimal risks and substantial potential benefits. As awareness grows and more research emerges, EECP treatment is likely to become an increasingly important component of comprehensive cardiovascular care.
If you or someone you know suffers from chronic angina or other cardiovascular symptoms that haven’t responded adequately to standard treatments, consider discussing EECP treatment with a healthcare provider to determine if this therapy might be appropriate.
About Vivek Sengar
Vivek Sengar is the founder of Fit My Heart and a leading expert in Non-Invasive and Preventive Cardiology. With over 11 years of clinical experience, he has helped thousands of patients avoid bypass surgery and stents through EECP Therapy, lifestyle changes, and natural heart care protocols. His mission is to make heart treatment safer, more effective, and surgery-free using globally accepted, evidence-based techniques.
Founder of Fit My Heart | Expert in Non-Surgical Heart Care

Frequently Asked Questions About EECP Treatment
Q: What does EECP stand for?
A: EECP stands for Enhanced External Counterpulsation, a non-invasive treatment for certain cardiovascular conditions.
Q: How does EECP therapy work?
A: EECP uses inflatable cuffs on the legs that synchronize with your heartbeat to improve blood flow to the heart by compressing during the heart’s resting phase.
Q: What conditions can EECP treat?
A: EECP primarily treats angina, coronary artery disease, heart failure, and can help patients who aren’t candidates for surgery or other interventions.
Q: How long is a typical EECP session?
A: Each EECP session typically lasts 1 hour, with patients usually receiving 35 sessions over a 7-week period.
Q: Is EECP therapy painful?
A: EECP is not painful, though some patients report a tight squeezing sensation. Most find it comfortable enough to read or nap during treatment.
Q: How soon can patients expect results from EECP?
A: Some patients notice improvement after 15-20 sessions, though maximum benefits are typically observed after completing the full course of treatment.
Q: How long do the benefits of EECP last?
A: Benefits typically last 2-5 years for most patients, with some experiencing relief for even longer periods.
Q: Who is not eligible for EECP treatment?
A: EECP is not recommended for patients with severe aortic insufficiency, recent cardiac catheterization, irregular heartbeats, or blood clotting issues.
Q: Does insurance cover EECP therapy?
A: In USA Many insurance plans, including Medicare, cover EECP therapy for patients with refractory angina who meet specific criteria, but in India getting the insurance cover is not easy but if there are no other option and your doctor is strongly recommonding you for EECP then some insurance companies may give the coverage under special health conditions.
Q: Can EECP replace bypass surgery or angioplasty?
A: It’s a Subjective question. In many cases, it can avoid the need for Bypass surgery, but EECP is not a replacement for these procedures, but serves as an alternative for patients who cannot undergo them or as complementary therapy.
Q: What side effects might occur with EECP?
A: Minor side effects may include skin irritation, muscle fatigue, or slight bruising. Serious side effects are extremely rare.
Q: Can I continue taking my medications during EECP treatment?
A: Yes, patients should continue their prescribed medications during EECP therapy unless directed otherwise by their physician.
Q: Is there any special preparation needed before an EECP session?
A: Wear comfortable, loose-fitting clothing, avoid heavy meals before treatment, and ensure proper hydration for optimal results.
Q: How is EECP different from a blood pressure cuff?
A: While both use compression, EECP uses multiple cuffs precisely synchronized with the heart cycle and delivers much stronger, sequential pressure.
Q: Can I resume normal activities after EECP therapy?
A: Yes, most patients can immediately resume normal daily activities, with many reporting increased energy and exercise capacity after completing treatment.
EECP Treatment for Chest Pain: Best Non Surgical Treatment for Coronary Blockages
Posted byEECP Treatment for Chest Pain: EECP treatment has emerged as one of the most promising non-invasive therapies for patients suffering from chronic angina and related cardiovascular conditions. Enhanced External Counterpulsation (EECP) treatment offers hope to those who have exhausted conventional treatment options. Despite being in clinical use for decades, many healthcare professionals remain unfamiliar with the detailed mechanisms of how EECP treatment delivers its therapeutic benefits. This comprehensive review examines the technical aspects of EECP treatment , its physiological effects on the cardiovascular system, and the complex signaling pathways that mediate its clinical outcomes.
Understanding EECP Treatment for Chest Pain
EECP treatment is a non-invasive, mechanical therapy approved by the FDA specifically for chronic stable angina that remains refractory to optimal anti-anginal medication and revascularization procedures. The EECP treatment involves the sequential inflation and deflation of pressure cuffs wrapped around the patient’s calves, thighs, and buttocks to create beneficial hemodynamic effects.
Technical Setup of EECP Treatment
The EECP treatment equipment consists of:
- Three pairs of pneumatic cuffs applied to the calves, lower thighs, and upper thighs/buttocks
- A computerized pneumatic control system
- An ECG monitoring system
- A finger plethysmograph to monitor arterial waveforms
During EECP treatment patients lie comfortably on a treatment table while the cuffs inflate and deflate in synchrony with their cardiac cycle. The timing for EECP treatment for chest pain is precisely controlled using the patient’s ECG signal:
- Diastole: During EECP treatment , the cuffs rapidly inflate sequentially from calves to thighs to buttocks, creating a retrograde pressure wave
- Systole: The cuffs simultaneously deflate, allowing the heart to pump against reduced vascular resistance
Each EECP treatment for chest pain session typically lasts 1 hour, with patients undergoing a standard course of 35 one-hour sessions over 7 weeks (5 sessions per week).
Hemodynamic Effects of EECP Treatment
The controlled application of external pressure during EECP treatment for chest pain produces several immediate hemodynamic effects:
Diastolic Augmentation During EECP Treatment for Chest Pain
During cuff inflation (diastole) in EECP treatment for chest pain, the retrograde pressure wave increases:
- Coronary perfusion pressure
- Coronary blood flow
- Venous return to the heart
- Cardiac output
Studies using Doppler echocardiography have demonstrated that EECP treatment for chest pain can increase diastolic coronary flow velocity by 28-30% in patients with coronary artery disease.
Systolic Unloading with EECP Treatment for Chest Pain
During cuff deflation (systole) in EECP treatment for chest pain, there is:
- Decreased peripheral vascular resistance
- Reduced cardiac afterload
- Decreased myocardial oxygen demand
- Improved left ventricular ejection fraction
This synchronized counterpulsation effect during EECP treatment for chest pain creates hemodynamics similar to those produced by intra-aortic balloon pump therapy, but without its invasive nature and associated risks.
Molecular and Cellular Mechanisms of EECP Treatment for Chest Pain
EECP treatment for chest pain triggers a cascade of biomolecular responses that extend far beyond its immediate hemodynamic effects. These responses involve complex signaling pathways affecting vascular endothelium, smooth muscle cells, and circulating progenitor cells.
Shear Stress and Endothelial Function in EECP Treatment for Chest Pain
The increased blood flow and pressure gradients generated by EECP treatment for chest pain create significant shear stress on the vascular endothelium. This mechanical force activates mechanoreceptors and initiates several signaling pathways:
- eNOS Activation: Shear stress during EECP treatment for chest pain phosphorylates endothelial nitric oxide synthase (eNOS) through the PI3K/Akt pathway, increasing nitric oxide (NO) production
- Mechanotransduction Pathways during EECP treatment:
- Activation of integrins and focal adhesion kinases
- Phosphorylation of PECAM-1 (Platelet Endothelial Cell Adhesion Molecule-1)
- Conformational changes in glycocalyx components
- Transcription Factor Regulation with EECP treatment:
- Increased nuclear translocation of Nrf2 (Nuclear factor erythroid 2-related factor 2)
- Reduced NF-κB (Nuclear Factor kappa B) activation
- Upregulation of KLF2 (Krüppel-like Factor 2), a flow-responsive transcription factor
Nitric Oxide Pathway in EECP Treatment for Chest Pain
Nitric oxide plays a central role in the mechanism of EECP treatment:
- Production: EECP treatment for chest pain increases eNOS activity, catalyzing the conversion of L-arginine to L-citrulline and NO
- Signaling during EECP treatment:
- NO diffuses to vascular smooth muscle cells
- Activates soluble guanylate cyclase (sGC)
- Increases intracellular cGMP levels
- Activates protein kinase G (PKG)
- PKG phosphorylates multiple targets, leading to reduced intracellular Ca²⁺ and smooth muscle relaxation
- Effects of EECP treatment:
- Vasodilation of existing vessels
- Anti-inflammatory actions
- Anti-platelet aggregation
- Inhibition of smooth muscle cell proliferation
- Reduction of leukocyte adhesion to endothelium
Research has demonstrated that EECP treatment for chest pain increases NO bioavailability, with studies showing elevated plasma nitrite/nitrate levels (stable NO metabolites) after a course of treatment.
Angiogenesis and Arteriogenesis with EECP Treatment for Chest Pain
EECP treatment for chest pain stimulates both angiogenesis (formation of new capillaries) and arteriogenesis (enlargement of pre-existing collateral vessels):
Angiogenic Pathways in EECP Treatment for Chest Pain
- VEGF Signaling:
- Increased shear stress during EECP treatment for chest pain upregulates Vascular Endothelial Growth Factor (VEGF) expression
- VEGF binds to VEGFR-2 on endothelial cells
- Activates PLCγ-PKC-MAPK pathway
- Stimulates endothelial cell proliferation and migration
- HIF-1α Pathway activation during EECP treatment:
- Shear stress stabilizes Hypoxia-Inducible Factor 1-alpha (HIF-1α)
- HIF-1α translocates to the nucleus
- Binds to Hypoxia Response Elements (HREs)
- Upregulates transcription of numerous angiogenic genes (VEGF, bFGF, PDGF)
- Other Proangiogenic Factors increased by EECP treatment:
- Increased expression of basic Fibroblast Growth Factor (bFGF)
- Elevated levels of Hepatocyte Growth Factor (HGF)
- Upregulation of angiopoietins (Ang-1 and Ang-2)
Arteriogenic Mechanisms of EECP Treatment for Chest Pain
- Fluid Shear Stress: The altered pressure gradients in EECP treatment for chest pain activate:
- Monocyte chemoattractant protein-1 (MCP-1) expression
- Granulocyte-macrophage colony-stimulating factor (GM-CSF) production
- Metalloproteinase Activation during EECP treatment:
- Increased expression of MMP-2 and MMP-9
- Breakdown of extracellular matrix to permit vessel expansion
- Remodeling of vascular architecture
- Growth Factor Signaling enhanced by EECP treatment:
- Platelet-Derived Growth Factor (PDGF) pathway activation
- Transforming Growth Factor-beta (TGF-β) signaling
- Upregulation of Fibroblast Growth Factor Receptor 1 (FGFR1)
Clinical evidence supports these mechanisms, with studies showing increased circulating levels of VEGF, bFGF, and HGF following EECP treatment for chest pain.
Progenitor Cell Mobilization in EECP Treatment for Chest Pain
EECP treatment for chest pain promotes the mobilization and homing of endothelial progenitor cells (EPCs) from bone marrow to sites of vascular injury:
- Mobilization Mechanisms during EECP treatment:
- Increased shear stress activates eNOS in bone marrow
- Elevated NO levels promote MMP-9 expression
- MMP-9 cleaves membrane-bound Kit ligand
- This releases soluble Kit ligand, which promotes stem cell mobility
- Homing Process enhanced by EECP treatment:
- Upregulation of SDF-1 (Stromal cell-Derived Factor-1) at sites of vascular stress
- SDF-1 binds to CXCR4 receptors on circulating EPCs
- This chemokine gradient directs EPCs to areas requiring vascular repair
- Differentiation during EECP treatment:
- Local factors promote EPC differentiation into mature endothelial cells
- Integration of these cells into the vascular wall
- Contribution to vascular repair and angiogenesis
Clinical studies have documented significant increases in circulating CD34+/KDR+ endothelial progenitor cells after EECP treatment for chest pain, supporting this mechanism.
Anti-inflammatory and Anti-oxidative Effects of EECP Treatment for Chest Pain
EECP treatment for chest pain exerts substantial anti-inflammatory effects:
- Reduced Inflammatory Markers with EECP treatment:
- Decreased C-reactive protein (CRP) levels
- Lower tumor necrosis factor-alpha (TNF-α) concentrations
- Reduced interleukin-6 (IL-6) and IL-1β
- Antioxidant Mechanisms activated by EECP treatment:
- Activation of Nrf2 pathway
- Upregulation of heme oxygenase-1 (HO-1)
- Increased superoxide dismutase (SOD) activity
- Elevated glutathione peroxidase expression
- Leukocyte Interaction modified by EECP treatment:
- Decreased expression of adhesion molecules (VCAM-1, ICAM-1, E-selectin)
- Reduced leukocyte rolling and adherence to endothelium
- Diminished neutrophil activation
Clinical Applications and Outcomes of EECP Treatment:
Refractory Angina
The primary indication for EECP treatment is chronic stable angina that remains symptomatic despite optimal medical therapy and revascularization. The International EECP Patient Registry reported that:
- 73-89% of patients undergoing EECP treatment experienced reduction in angina by at least one Canadian Cardiovascular Society (CCS) class
- 50% reduction in nitroglycerin use after EECP treatment
- Significant improvement in quality of life measures with EECP treatment
- Benefits of EECP treatment persisting for 3-5 years after treatment in many patients
Heart Failure Management with EECP Treatment:
Growing evidence supports the efficacy of EECP treatment in heart failure with reduced ejection fraction:
- The PEECH trial (Prospective Evaluation of EECP in Congestive Heart Failure) demonstrated that EECP treatment provides:
- Improved exercise tolerance
- Enhanced quality of life
- Increased peak oxygen consumption
- Reduced B-type natriuretic peptide (BNP) levels
- Proposed mechanisms of EECP treatment in heart failure include:
- Improved endothelial function
- Enhanced peripheral perfusion
- Reduced systemic vascular resistance
- Decreased left ventricular wall stress
- Improved coronary perfusion
Other Applications of EECP Treatment:
Emerging research suggests potential benefits of EECP treatment in:
- Cardiac syndrome X (microvascular dysfunction)
- Peripheral arterial disease
- Post-cardiac transplantation allograft vasculopathy
- Erectile dysfunction of vascular origin
- Restless leg syndrome
- Acute ischemic stroke
Limitations and Contraindications for EECP Treatment:
Despite its impressive safety profile, EECP treatment is contraindicated in certain conditions:
- Coagulopathy with INR > 2.5
- Arrhythmias interfering with ECG triggering
- Active thrombophlebitis
- Severe peripheral arterial disease
- Aortic aneurysm requiring surgical repair
- Pregnancy
- Severe aortic insufficiency (relative contraindication)
Future Directions for EECP Treatment:
Current research in EECP treatment is exploring several exciting directions:
- Optimized Treatment Protocols: Investigating whether modified EECP treatment schedules or pressure patterns might enhance outcomes for specific patient populations
- Biomarker-Guided Therapy: Development of biomarker panels to identify patients most likely to benefit from EECP treatment
- Combination Approaches: Evaluating EECP treatment in combination with stem cell therapy, gene therapy, or novel pharmacological agents
- Expanded Applications: Testing EECP treatment in cerebrovascular disease, venous insufficiency, and metabolic disorders
- Mechanistic Research: Further elucidation of the molecular pathways and genetic modulators that mediate the effects of EECP treatment
Conclusion
EECP treatment for chest pain represents a sophisticated, non-invasive therapeutic approach for patients with refractory angina and potentially other cardiovascular conditions. The mechanism of EECP treatment extends far beyond simple hemodynamic effects, encompassing complex cellular and molecular pathways that promote vascular health and myocardial perfusion.
As our understanding of EECP treatment continues to evolve, its clinical applications will likely expand and patient selection will improve in the coming years. For patients who have exhausted conventional treatment options, EECP treatment offers a safe, effective alternative that addresses not just the symptoms but the underlying vascular pathophysiology of ischemic heart disease.
Healthcare is increasingly moving toward less invasive, more physiologically-based interventions, and EECP treatment stands as a prime example of how mechanical therapies can harness and enhance the body’s natural healing processes without the risks associated with invasive procedures.
About Vivek Sengar
Vivek Sengar is the founder of Fit My Heart and a leading expert in Non-Invasive and Preventive Cardiology. With over 11 years of clinical experience, he has helped thousands of patients avoid bypass surgery and stents through EECP Therapy, lifestyle changes, and natural heart care protocols. His mission is to make heart treatment safer, more effective, and surgery-free using globally accepted, evidence-based techniques.
Founder of Fit My Heart | Expert in Non-Surgical Heart Care
✅ Get a Second Opinion on Chest Pain or Blockages
✅ Know if EECP is Right for You
15 Frequently Asked Questions About EECP Treatment for Chest Pain
Que: What exactly is EECP therapy?
Ans: EECP (Enhanced External Counterpulsation) is a non-invasive, FDA-approved therapy that uses inflatable cuffs on the legs to increase blood flow to the heart, effectively reducing chest pain in patients with chronic angina.
Que: How does the EECP mechanism work for angina relief?
Ans: EECP works through timed, sequential inflation of leg cuffs during diastole, pushing blood back to the heart, which improves coronary blood flow and reduces angina symptoms.
Que: Who qualifies as an ideal candidate for this treatment?
Ans: Patients with chronic, stable angina who haven’t responded adequately to medication and aren’t candidates for invasive procedures like stenting or bypass surgery are ideal candidates for EECP therapy.
Que: How long does a typical EECP session last?
Ans: Each EECP session typically lasts one hour, with patients usually receiving 35 sessions over a 7-week period (5 sessions per week).
Que: Is the EECP procedure painful?
Ans: No, EECP is not painful. Most patients report feeling pressure similar to a firm massage on their legs during treatment, but not pain.
Que: What are the success rates of EECP for treating angina?
Ans: Clinical studies show 70-80% of patients experience significant reduction in angina symptoms, with benefits often lasting 3-5 years after completing treatment.
Que: How does EECP compare to angioplasty or stents?
Ans: Unlike invasive procedures, EECP is completely non-invasive with no recovery time. It works by improving overall circulation rather than treating specific blockages.
Que: What are the potential side effects of this therapy?
Ans: Side effects are minimal and may include mild skin irritation, muscle fatigue, or leg discomfort. Serious complications are extremely rare.
Que: How soon will I notice results from the treatment?
Ans: Many patients report improvement in chest pain symptoms after 15-20 sessions, though the full benefits typically manifest after completing the 35-session protocol.
Que: Is EECP therapy covered by insurance?
Ans: Most insurance plans, including Medicare, cover EECP for angina patients who meet specific criteria for refractory angina.
Que: Can EECP help conditions other than chest pain?
Ans: Yes, emerging research suggests EECP may benefit heart failure, peripheral artery disease, erectile dysfunction, and some forms of stroke.
Que: How does EECP stimulate new blood vessel growth?
Ans: EECP increases shear stress on vessel walls, activating growth factors like VEGF and HIF-1α that promote angiogenesis (new capillary formation) and arteriogenesis (collateral vessel enlargement).
Que: Who should avoid this treatment?
Ans: EECP is contraindicated for patients with severe coagulopathy, arrhythmias, active thrombophlebitis, severe peripheral arterial disease, aortic aneurysm, pregnancy, or severe aortic insufficiency.
Que: Can I maintain normal activities during my EECP course?
Ans: Yes, most patients can maintain their normal daily activities during the treatment period. There’s no downtime or recovery period after individual sessions.
Que: Should I continue taking my medications during EECP therapy?
Ans: Yes, patients should continue taking prescribed medications during EECP. Some patients may require less medication after completing treatment, but changes should only be made under doctor supervision.
Enhanced External Counterpulsation: 3 Unique Benefits of EECP
Posted byEnhanced External Counterpulsation: What is EECP?
-
EECP (Enhanced External Counterpulsation) is a non-invasive circulatory support technique.
-
It uses inflatable cuffs (like blood pressure cuffs) placed on the legs and buttocks.
-
The cuffs inflate and deflate in sync with the heartbeat, improving blood flow to the heart, brain, and other vital organs.
-
It enhances circulation by increasing venous return and diastolic aortic pressure, which improves myocardial function.
How Does Enhanced External Counterpulsation (EECP) Work?
-
Sequential inflation of the cuffs squeezes blood from the legs toward the heart.
-
The inflation occurs during the heart’s resting phase (diastole) to boost blood supply.
-
It helps open smaller blood vessels, reduces inflammation, and supports vessel repair.
-
Benefits include:
-
Increased blood flow to vital organs (heart, brain, kidneys)
-
Improved heart function and reduced stress
-
Support for brain recovery after stroke
-
Better blood sugar control in diabetics
-
Who Can Benefit from Enhanced External Counterpulsation EECP?
EECP is especially helpful for patients with the following conditions:
-
Cardiovascular Issues:
-
Angina (chest pain)
-
Heart failure
-
Past heart attacks
-
-
Neurological Disorders:
-
Ischemic stroke
-
Parkinson’s disease
-
Alzheimer’s disease
-
-
Metabolic and Other Conditions:
-
Type 2 diabetes (and its complications)
-
Eye diseases due to poor blood flow
-
Sleep disorders
-
Erectile dysfunction
-
Sudden hearing loss
-
Depression or anxiety due to chronic illness
-
Also Read: EECP Treatment for Old Age Patients
Who Should Not Receive EECP? (Contraindications)
-
Blood clots in the legs
-
Severe heart valve problems (e.g., severe aortic regurgitation)
-
Uncontrolled high blood pressure
-
Irregular heartbeat not well-managed
-
Open wounds or skin infections on the legs
-
High lung pressure
How is EECP Administered?
-
Standard Protocol:
-
1 hour/day, 5–6 days/week for 6–7 weeks (total of 35–36 hours)
-
-
Cuffs are placed on:
-
Calves
-
Thighs
-
Buttocks
-
-
Monitoring includes:
-
Blood pressure
-
Heart rate and rhythm
-
Oxygen saturation
-
Skin condition
-
-
Adjustments:
-
Based on patient comfort and response
-
Treatment stopped if oxygen drops or pain occurs
-
How to Prepare for EECP
-
Keep stomach empty for at least 2–3 hours before the session
-
Empty your bladder for comfort before starting
-
Take prescribed medications as advised by your doctor
-
Wear loose, comfortable clothing; avoid tight undergarments
-
Avoid caffeine or heavy meals right before treatment
-
Stay relaxed and calm; deep breathing may help
-
Avoid using mobile phones or talking during the session
-
Inform staff if you feel discomfort, pain, dizziness, or shortness of breath
-
Remove jewelry or objects around waist and thighs
-
Bring water and a light snack for after the session if needed
Safety and Monitoring
-
Patients should be screened before starting EECP.
-
Ongoing monitoring during sessions is essential.
-
Doctors adjust cuff pressure and timing as needed.
-
EECP is generally safe and well-tolerated with proper care.
Treatment Maintenance and Follow-up
-
Shorter sessions can be used for less fit or frail patients.
-
Booster treatments can be repeated yearly.
-
Maintenance therapy may include 2–3 hours/week after initial cycle.
Benefits of EECP
-
Reduces chest pain and improves exercise tolerance
-
Enhances heart and brain function
-
Supports recovery after heart procedures or stroke
-
Improves quality of life in elderly patients
-
Helps manage:
-
Sleep and mood disorders
-
Blood sugar in diabetics
-
Vision and hearing loss
-
Sexual dysfunction
-
Conclusion
EECP is a safe, non-invasive, and effective treatment option for elderly individuals with cardiovascular, neurological, and metabolic conditions. It is especially valuable for those who are not good candidates for surgery or strong medications. With proper screening, individualized protocols, and professional monitoring, EECP significantly improves symptoms, functionality, and overall quality of life.
About Mr. Vivek Singh Sengar
Mr. Vivek Singh Sengar is a highly respected EECP (Enhanced External Counterpulsation) expert with over 13 years of clinical experience in the field of non-invasive cardiology and integrative care. As the Founder of FIT MY HEART, he has dedicated his career to providing advanced EECP therapy to patients suffering from chronic heart conditions such as heart failure, angina, low ejection fraction, post-heart attack recovery, and coronary blockages.
Trained in Clinical Nutrition and Integrative Cardiac Rehabilitation, Mr. Sengar blends modern science with lifestyle medicine to deliver holistic, drug-free heart care. He has treated thousands of patients who were either ineligible for bypass or angioplasty, helping them regain functional capacity, improve heart pumping, and reverse symptoms—often without surgery.
His approach combines EECP with chrono-nutrition, therapeutic fasting, herbal support, Panchakarma, and patient education to address root causes rather than just symptoms. Mr. Sengar is also the creator of India’s first 60-hour EECP training program for healthcare professionals and is widely regarded as a pioneer in the expansion of EECP in India for both cardiac and non-cardiac applications.
With a deep passion for preventive healthcare, Mr. Vivek Singh Sengar continues to inspire trust, transformation, and long-term wellness in patients across the country.
