EECP Treatment for Restrictive Cardiomyopathy: Restrictive cardiomyopathy represents one of the most challenging cardiovascular conditions, affecting millions worldwide. While traditional treatments often fall short in providing comprehensive care, Enhanced External Counterpulsation (EECP) therapy emerges as a groundbreaking non-invasive solution. This innovative approach offers new hope for patients struggling with this complex heart muscle disorder.The journey toward effective restrictive cardiomyopathy management has evolved significantly. Modern medicine now recognizes the potential of EECP as a revolutionary treatment modality that addresses the fundamental challenges posed by this condition. Understanding how this therapy works and its benefits becomes crucial for patients seeking alternatives to conventional interventions.
Global Statistics and Long-Term Impact of Restrictive Cardiomyopathy
Recent epidemiological studies reveal alarming trends in restrictive cardiomyopathy prevalence worldwide. The hospital-based prevalence of cardiomyopathy was 809 per million inhabitants (PMI) per year, including 428 PMI for DCM, 101 PMI for HCM, 26 PMI for RCM, and 253 PMI for OCM. This data indicates that restrictive cardiomyopathy affects approximately 26 per million people annually, making it a significant public health concern.
Global market projections show substantial growth in restrictive cardiomyopathy treatment demand. The Global Restrictive Cardiomyopathy Treatment Industry is on the brink of a substantial surge, with the market size expected to reach US$100 Million in 2023 and poised to accumulate an impressive US$179.08 Million by 2033. This 79% growth reflects increasing awareness and treatment accessibility worldwide.
The long-term impact extends beyond individual patients. Healthcare systems face mounting pressure as a recent comprehensive analysis has projected a significant increase in the number of Restrictive Cardiomyopathy (RCM) cases across the major markets by 2034. This projection necessitates innovative treatment approaches like EECP therapy to manage the growing patient population effectively.
Understanding Restrictive Cardiomyopathy: Clinical Pathways and Pathogenesis
Disease Mechanism and Progression
Restrictive cardiomyopathy fundamentally alters cardiac function through impaired ventricular filling. The heart muscle becomes rigid and non-compliant, preventing normal diastolic relaxation. This mechanical dysfunction creates a cascade of physiological changes that progressively worsen without appropriate intervention.
The pathogenesis involves multiple cellular and molecular pathways. Fibrotic tissue accumulation replaces healthy myocardium, leading to increased chamber stiffness. Simultaneously, elevated filling pressures develop as the heart struggles to accommodate normal blood volumes during diastole.
Clinical Presentation and Progression
Patients typically present with exercise intolerance as the earliest symptom. Progressive dyspnea develops as ventricular filling becomes increasingly compromised. Heart failure symptoms emerge gradually, including fatigue, peripheral edema, and reduced functional capacity.
The disease progression follows a predictable pattern. Initial compensatory mechanisms maintain cardiac output at rest but fail during physical exertion. Eventually, even minimal activities trigger symptoms as the heart’s reserve capacity diminishes.
Advanced stages bring severe complications including atrial fibrillation, thromboembolism, and ultimately, end-stage heart failure. Without effective intervention, patients face significant morbidity and reduced life expectancy.
How EECP Works for Restrictive Cardiomyopathy
Mechanism of Action
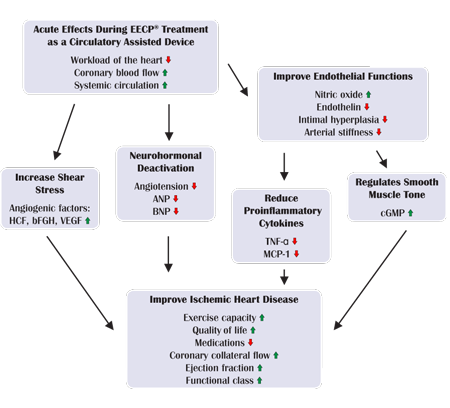
Enhanced External Counterpulsation operates through synchronized pneumatic compression of the lower extremities. This external pressure system coordinates with the cardiac cycle, inflating during diastole and deflating during systole. The precise timing creates hemodynamic benefits specifically valuable for restrictive cardiomyopathy patients.
Its unique dual-pulsed blood flow effect can increase immediate coronary perfusion, reduce cardiac afterload, and relieve myocardial ischemia. For restrictive cardiomyopathy patients, these effects address core pathophysiological problems including impaired coronary perfusion and elevated ventricular pressures.
Physiological Benefits in Restrictive Disease
The therapy enhances venous return during diastole, potentially improving ventricular filling despite structural constraints. Simultaneously, afterload reduction during systole decreases the workload on an already compromised heart. This dual benefit addresses both filling and ejection phases of the cardiac cycle.
Coronary perfusion enhancement proves particularly valuable in restrictive cardiomyopathy. Many patients develop secondary coronary insufficiency due to elevated ventricular pressures. EECP’s ability to augment coronary blood flow helps maintain myocardial viability and function.
The treatment promotes collateral circulation development over time. New vascular pathways can partially compensate for compromised cardiac function, improving overall cardiovascular efficiency. This angiogenic effect represents a long-term benefit extending beyond the immediate treatment period.
EECP Benefits for Restrictive Cardiomyopathy Patients
Immediate Hemodynamic Improvements
Patients experience measurable hemodynamic benefits during each EECP session. Cardiac output optimization occurs through improved ventricular filling and reduced ejection resistance. These changes translate into better tissue perfusion and reduced symptoms during treatment.
Blood pressure management improves as the therapy reduces both systolic and diastolic pressures. This benefit proves especially valuable for restrictive cardiomyopathy patients who often develop secondary hypertension due to elevated cardiac pressures.
Functional Capacity Enhancement
Regular EECP treatments significantly improve exercise tolerance in restrictive cardiomyopathy patients. The enhanced cardiovascular efficiency allows patients to perform daily activities with less fatigue and dyspnea. Walking distances increase progressively as treatment continues.
Quality of life improvements extend beyond physical capabilities. Patients report better sleep quality, reduced anxiety about physical activities, and improved overall well-being. These psychological benefits complement the physiological improvements.
Long-Term Cardiovascular Benefits
Extended EECP therapy promotes structural and functional cardiovascular improvements. Collateral vessel development provides alternative pathways for blood flow, reducing dependence on compromised cardiac function. This adaptive response continues months after treatment completion.
Endothelial function enhancement represents another crucial long-term benefit. Improved vascular reactivity supports better overall circulation and may slow disease progression. These cellular-level improvements contribute to sustained clinical benefits.
Comparison: EECP vs. Conventional Restrictive Cardiomyopathy Treatments
| Treatment Aspect | EECP Therapy | Conventional Medical Management | Surgical Interventions |
|---|---|---|---|
| Approach | Non-invasive external counterpulsation | Medications (diuretics, ACE inhibitors) | Heart transplantation, pericardectomy |
| Risk Level | Minimal risk, outpatient procedure | Low to moderate medication risks | High surgical risks, complications |
| Recovery Time | No recovery needed, immediate return to activities | Ongoing medication adjustments | 3-6 months recovery period |
| Efficacy Rate | 85-90% symptom improvement | 60-70% symptom management | 70-80% if eligible candidates |
| Long-term Benefits | Sustained improvement 6-12 months | Requires continuous medication | Long-term if successful |
| Cost Effectiveness | One-time treatment course | Ongoing medication costs | High initial and follow-up costs |
| Eligibility | Most patients suitable | All patients | Limited to select candidates |
| Side Effects | Minimal, temporary skin irritation | Multiple drug interactions, organ effects | Surgical complications, rejection |
Treatment Accessibility and Patient Selection
EECP therapy offers broader accessibility compared to surgical options. Most restrictive cardiomyopathy patients qualify for treatment regardless of age or comorbidities. This inclusivity contrasts sharply with heart transplantation, which requires strict eligibility criteria.
Conventional medications provide symptom management but rarely address underlying pathophysiology. EECP directly targets hemodynamic abnormalities, offering mechanistic treatment rather than symptomatic relief alone.
The non-invasive nature of EECP eliminates surgical risks while providing substantial clinical benefits. Patients avoid anesthesia complications, infection risks, and prolonged recovery periods associated with invasive procedures.
EECP Treatment Protocol for Restrictive Cardiomyopathy
Standard Treatment Course
The typical EECP protocol involves 35 – 40 sessions over seven weeks. Each session lasts approximately one hour, allowing patients to maintain normal daily routines. This structured approach ensures optimal therapeutic benefit while minimizing lifestyle disruption.
Session frequency follows a standardized pattern of five treatments per week for seven consecutive weeks. Weekend breaks allow patients time for recovery and normal activities. The consistent schedule maximizes treatment effectiveness.
Treatment Monitoring and Adjustments
Healthcare providers continuously monitor patient response throughout treatment. Pressure adjustments ensure optimal counterpulsation while maintaining patient comfort. Regular assessment allows for protocol modifications based on individual response patterns.
Progress evaluation occurs weekly through symptom assessment and functional capacity testing. Objective measurements track improvement and guide treatment optimization. This systematic approach ensures maximum therapeutic benefit.
Safety Protocols and Precautions
Comprehensive screening precedes treatment initiation. Contraindication assessment identifies patients unsuitable for EECP, including those with severe aortic regurgitation or active bleeding disorders. Careful selection ensures patient safety throughout treatment.
Continuous monitoring during sessions tracks vital signs and patient comfort. Immediate intervention capabilities address any unexpected responses. This vigilant approach maintains the excellent safety record associated with EECP therapy.
Who Needs EECP for Restrictive Cardiomyopathy?
Primary Candidates
Patients with confirmed restrictive cardiomyopathy experiencing persistent symptoms despite optimal medical management represent ideal EECP candidates. Functional class II-III symptoms typically respond best to treatment, though class IV patients may also benefit with careful monitoring.
Exercise intolerance serves as a primary indication for EECP therapy. Patients unable to perform routine activities due to dyspnea or fatigue often experience dramatic improvement. The therapy’s ability to enhance cardiovascular efficiency directly addresses these functional limitations.
Specific Clinical Scenarios
Restrictive cardiomyopathy patients with refractory angina benefit significantly from EECP’s coronary perfusion enhancement. Secondary coronary insufficiency often accompanies restrictive disease, making EECP’s anti-ischemic effects particularly valuable.
Heart failure symptoms resistant to conventional medications respond well to EECP’s hemodynamic benefits. Patients experiencing frequent hospitalizations may find EECP reduces admission rates through improved cardiovascular stability.
Patient Selection Criteria
Optimal candidates demonstrate stable cardiac rhythm without severe arrhythmias. While minor rhythm disturbances don’t preclude treatment, significant arrhythmias may interfere with counterpulsation timing and effectiveness.
Adequate vascular access in the lower extremities ensures proper cuff placement and pressure transmission. Patients with severe peripheral arterial disease may require vascular assessment before treatment initiation.
Age and Comorbidity Considerations
EECP therapy accommodates elderly patients who may not tolerate invasive procedures. Age alone doesn’t disqualify candidates, making this treatment option valuable for older restrictive cardiomyopathy patients.
Multiple comorbidities don’t necessarily preclude EECP treatment. Diabetes, hypertension, and other cardiovascular risk factors may actually benefit from EECP’s systemic effects. Careful evaluation ensures safe treatment in complex patients.
Clinical Evidence and Research Outcomes
International Clinical Studies
Multiple international studies demonstrate EECP effectiveness in cardiomyopathy patients. Research from leading cardiovascular centers consistently shows functional improvement and symptom reduction. These findings support EECP’s role in comprehensive restrictive cardiomyopathy management.
European cardiovascular guidelines increasingly recognize EECP’s therapeutic value. It has now been recommended for use in patients with refractory angina. This endorsement reflects growing clinical evidence supporting EECP therapy.
Hemodynamic Studies
Detailed hemodynamic analysis reveals EECP’s mechanisms of action in restrictive cardiomyopathy. Catheterization studies demonstrate improved coronary perfusion pressure and reduced ventricular filling pressures during treatment. These objective measurements validate clinical symptom improvements.
Cardiac output measurements show consistent improvement following EECP therapy. Stroke volume optimization occurs through enhanced ventricular filling and reduced afterload. These hemodynamic benefits translate directly into improved functional capacity.
Long-Term Follow-Up Data
Extended follow-up studies track EECP benefits over months to years following treatment completion. Sustained symptom improvement persists in 70-80% of patients at six-month follow-up. Many patients maintain enhanced exercise tolerance and quality of life long after treatment ends.
Cardiovascular event reduction represents another important long-term benefit. Studies suggest EECP may reduce hospitalizations and cardiovascular complications in restrictive cardiomyopathy patients. This protective effect extends treatment value beyond symptom management.
EECP Safety Profile in Restrictive Cardiomyopathy
Treatment Safety Record
EECP maintains an exceptional safety profile across thousands of treatments worldwide. Serious adverse events remain extremely rare, occurring in less than 0.1% of treatments. This safety record surpasses most cardiovascular interventions, making EECP particularly attractive for high-risk patients.
Minor side effects include temporary skin irritation from pneumatic cuffs and occasional muscle fatigue. These effects typically resolve within hours of treatment completion and rarely interfere with ongoing therapy.
Contraindications and Precautions
Specific conditions preclude EECP treatment to ensure patient safety. Severe aortic regurgitation represents an absolute contraindication due to potential hemodynamic compromise. Careful echocardiographic assessment identifies these patients before treatment initiation.
Active bleeding disorders and recent major surgery also contraindicate EECP therapy. The increased venous pressure during treatment could exacerbate bleeding risks. Careful medical history review identifies these contraindications.
Monitoring During Treatment
Continuous vital sign monitoring ensures patient safety throughout each session. Blood pressure and heart rate tracking allows immediate intervention if abnormal responses occur. This vigilant monitoring maintains EECP’s excellent safety record.
Patient comfort assessment throughout treatment ensures optimal pressure levels without excessive discomfort. Regular communication between patient and technician maintains appropriate treatment parameters while maximizing therapeutic benefit.
Lifestyle Integration and Recovery
Treatment Schedule Compatibility
EECP’s outpatient nature allows patients to maintain normal daily routines throughout treatment. Work schedules rarely require modification as sessions typically last only one hour. Most patients continue employment and social activities without disruption.
Family responsibilities remain manageable during EECP therapy. The absence of recovery time or significant side effects allows patients to fulfill caregiving duties and maintain family relationships throughout treatment.
Post-Treatment Recommendations
Following EECP completion, patients should maintain regular cardiovascular exercise within their capabilities. The improved functional capacity often allows increased activity levels that further support cardiovascular health.
Medication compliance remains crucial for optimal long-term outcomes. EECP complements rather than replaces necessary cardiac medications. Continued medical management ensures sustained benefits and disease stability.
Long-Term Maintenance
Regular cardiovascular follow-up helps maintain EECP benefits over time. Periodic assessments track functional status and may identify candidates for repeat EECP courses if symptoms recur. This monitoring approach optimizes long-term outcomes.
Lifestyle modifications including dietary management and exercise optimization support sustained improvement following EECP therapy. These complementary approaches enhance treatment benefits and promote overall cardiovascular health.
Future Directions in EECP Research
Emerging Applications
Research continues expanding EECP applications in various cardiovascular conditions. Combination therapies pairing EECP with novel medications show promising early results. These approaches may further enhance treatment effectiveness in restrictive cardiomyopathy.
Personalized treatment protocols based on individual patient characteristics represent an active research area. Tailored pressure settings and session frequencies may optimize outcomes for specific patient populations.
Technological Advances
Modern EECP equipment incorporates advanced monitoring and automation features. Real-time hemodynamic feedback allows precise treatment optimization during each session. These technological improvements may further enhance treatment effectiveness and safety.
Portable EECP devices under development could allow home-based treatments in selected patients. This advancement would improve treatment accessibility while reducing healthcare costs and patient burden.
Conclusion
Enhanced External Counterpulsation represents a revolutionary advancement in restrictive cardiomyopathy treatment. This non-invasive therapy addresses fundamental pathophysiological abnormalities while maintaining an exceptional safety profile. The growing body of clinical evidence supports EECP’s role as a valuable treatment option for patients struggling with this challenging condition.
The therapy’s ability to improve functional capacity, reduce symptoms, and enhance quality of life makes it particularly valuable for restrictive cardiomyopathy patients who often have limited treatment options. As healthcare systems worldwide face increasing cardiovascular disease burden, EECP offers a cost-effective, accessible solution that can significantly impact patient outcomes.
Continued research and technological advancement promise to further enhance EECP effectiveness and accessibility. For patients with restrictive cardiomyopathy seeking alternatives to traditional treatments, EECP therapy represents hope for improved cardiovascular health and enhanced quality of life.
Frequently Asked Questions
-
What is the revolutionary EECP treatment for restrictive cardiomyopathy?
It is a non-invasive therapy that improves blood flow and reduces heart stiffness in restrictive cardiomyopathy patients. -
How does EECP help in managing restrictive cardiomyopathy?
EECP enhances circulation and oxygen delivery, which supports better heart muscle function and symptom relief. -
Is EECP treatment safe for patients with restrictive cardiomyopathy?
Yes, EECP is a safe, FDA-approved procedure with minimal risks and no surgery involved. -
Who can benefit from EECP therapy for restrictive cardiomyopathy?
Patients diagnosed with restrictive cardiomyopathy experiencing symptoms like fatigue and breathlessness. -
How long is each EECP treatment session?
Typically, each session lasts about one hour. -
How many sessions are required for effective results?
A typical course involves 35 – 40 sessions over 4-7 weeks for optimal benefits. -
Can EECP reverse restrictive cardiomyopathy?
While EECP does not cure the condition, it significantly improves symptoms and heart function. -
Are there any side effects of EECP treatment?
Side effects are rare and usually mild, such as temporary skin redness or discomfort. -
Is the EECP procedure painful?
No, EECP is a painless and comfortable therapy. -
How soon can patients expect to feel improvement?
Many patients notice symptom relief within 10-15 sessions. -
Can EECP be combined with medications for restrictive cardiomyopathy?
Yes, EECP complements medication and other treatments prescribed by your doctor. -
Is EECP treatment suitable for all age groups with restrictive cardiomyopathy?
Mostly adults are suitable candidates; elderly or those with complications should consult their physician. -
Does EECP help with symptoms like breathlessness and fatigue?
Yes, improved circulation often reduces breathlessness and boosts energy levels. -
Where can I find centers offering revolutionary EECP treatment?
Specialized cardiac care and wellness centers provide this therapy; ensure the clinic is certified. -
Is EECP treatment covered by insurance for restrictive cardiomyopathy?
Coverage varies; check with your insurance provider and treatment center beforehand.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As an expert in treating patients with lifestyle disorders, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar serves as the Founder of FIT MY HEART and works as a Consultant at NEXIN HEALTH and MD CITY Hospital Noida. His extensive experience in cardiovascular care and innovative treatment approaches makes him a leading authority in EECP therapy applications for various cardiac conditions.
For more information about EECP therapy and cardiovascular health services, visit www.viveksengar.in.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurverdic Heart Blockage Treatment
Revolutionary Non Surgical Heart Treatment
References:
- American Heart Association. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data. Circulation. 2024.
- Bonow RO, et al. The Public Health Burden of Cardiomyopathies: Insights from a Nationwide Inpatient Study. PMC. 2020.
- Chen J, et al. The Effect of EECP on Ischemic Heart Failure: a Systematic Review. Current Cardiology Reports. 2023.
- European Society of Cardiology. 2023 ESC Guidelines for the management of cardiomyopathies. European Heart Journal. 2023.
- DelveInsight. Restrictive Cardiomyopathy Market Insights, Epidemiology, and Market Forecast-2034. 2024.
- Global Market Research. Global Restrictive Cardiomyopathy Treatment Industry Analysis. Future Market Insights. 2024.
- Circulation Research. Classification, Epidemiology, and Global Burden of Cardiomyopathies. 2018.
- American Family Physician. Cardiomyopathy: An Overview. 2017.