EECP Treatment for Dilated Cardiomyopathy: Dilated cardiomyopathy represents one of the most challenging heart conditions affecting millions worldwide. While traditional treatments often involve invasive procedures or medications with significant side effects, Enhanced External Counterpulsation (EECP) emerges as a groundbreaking non-invasive therapy. This innovative approach offers hope to patients seeking alternatives to conventional cardiac interventions.Modern cardiology has witnessed remarkable advances in treating complex heart conditions. EECP therapy stands out as a revolutionary treatment modality that addresses the underlying pathophysiology of dilated cardiomyopathy without requiring surgical intervention. Understanding how this therapy works and its benefits can help patients make informed decisions about their cardiac care.
Global Statistics and Long-Term Impact of Dilated Cardiomyopathy
Dilated cardiomyopathy affects approximately 36 out of every 100,000 individuals globally, making it one of the most prevalent forms of cardiomyopathy. The clinical incidence is 2.45 cases per 100,000 population per year, while autopsy studies reveal higher rates, suggesting many cases remain undiagnosed during life.
The mortality statistics paint a sobering picture of this condition’s severity. Research shows a 55.9% mortality rate in the first five years, and a 65.8% mortality rate at 15 years. These figures highlight the urgent need for effective treatment strategies that can improve both quality of life and long-term survival rates.
Heart failure statistics reveal that dilated cardiomyopathy contributes significantly to global cardiovascular mortality. The economic burden extends beyond immediate medical costs, encompassing reduced productivity, frequent hospitalizations, and long-term care requirements. Families often face emotional and financial stress as they navigate this chronic condition.
Progressive nature of dilated cardiomyopathy means early intervention becomes crucial. Patients who receive timely and appropriate treatment show better outcomes compared to those whose condition advances to end-stage heart failure. This reality emphasizes the importance of exploring all available therapeutic options, including innovative approaches like EECP therapy.
Understanding Dilated Cardiomyopathy: Clinical Pathways and Pathogenesis
Dilated cardiomyopathy fundamentally involves the enlargement and weakening of the heart’s main pumping chamber. This clinical diagnosis is characterized by left ventricular or biventricular dilation and impaired contraction that is not explained by abnormal loading conditions or coronary artery disease. The condition represents a complex interplay of genetic, environmental, and lifestyle factors.
Pathogenetic Mechanisms
The pathogenesis of dilated cardiomyopathy involves multiple interconnected pathways. Genetic mutations affecting sarcomere proteins, desmosome components, and ion channels can trigger the disease process. Environmental factors such as viral infections, toxins, and autoimmune responses contribute to myocardial damage and subsequent remodeling.
Molecular mechanisms underlying dilated cardiomyopathy include altered calcium handling, impaired energy metabolism, and disrupted protein synthesis. These changes lead to progressive myocyte loss, fibrosis development, and ventricular remodeling. Understanding these pathways helps explain why comprehensive treatment approaches often yield better results than single-target therapies.
Disease Progression Patterns
Early stages of dilated cardiomyopathy may present with subtle symptoms or remain asymptomatic. Compensatory mechanisms initially maintain cardiac output despite reduced contractility. However, these adaptations eventually become maladaptive, leading to further deterioration.
Progressive ventricular dilation occurs as the heart attempts to maintain stroke volume despite decreased contractile function. This compensatory mechanism initially preserves cardiac output but ultimately leads to increased wall stress, further myocardial damage, and activation of neurohormonal systems that perpetuate the disease process.
Advanced stages manifest with clinical heart failure symptoms including dyspnea, fatigue, and exercise intolerance. Arrhythmias become more common as the electrical conduction system becomes affected by structural changes. Without appropriate intervention, the condition progresses to end-stage heart failure requiring advanced therapies.
How EECP Treatment Works for Dilated Cardiomyopathy
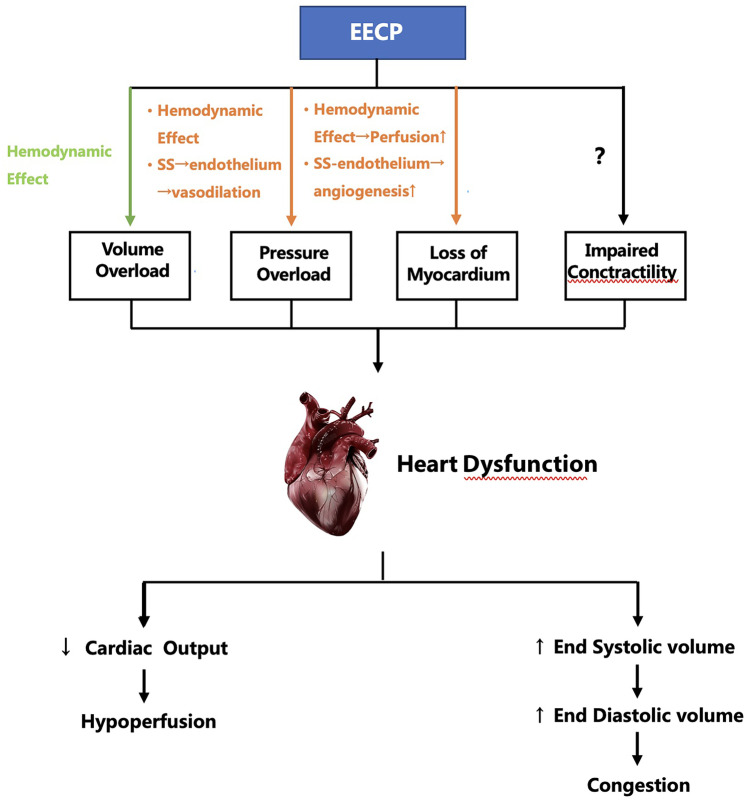
Enhanced External Counterpulsation operates on sophisticated hemodynamic principles that directly address the pathophysiology of dilated cardiomyopathy. The therapy involves sequential inflation and deflation of cuffs wrapped around the patient’s legs, synchronized with the cardiac cycle to optimize blood flow patterns.
Mechanism of Action
EECP therapy creates a secondary circulation system that augments diastolic pressure while reducing systolic afterload. By promoting venous return and decreasing afterload, EECP can decrease oxygen consumption and enhance cardiac output by up to 25%. This dual effect addresses two critical issues in dilated cardiomyopathy: inadequate coronary perfusion and excessive cardiac workload.
During diastole, cuff inflation enhances coronary perfusion pressure, improving oxygen delivery to compromised myocardium. Simultaneously, rapid cuff deflation during systole reduces afterload, allowing the weakened heart to pump more efficiently. This mechanism directly counteracts the hemodynamic abnormalities characteristic of dilated cardiomyopathy.
Physiological Benefits
The therapy promotes coronary collateral development through enhanced shear stress and growth factor activation. New blood vessel formation improves myocardial perfusion in areas with compromised circulation. This angiogenic effect provides long-term benefits beyond the immediate hemodynamic improvements.
Neurohormonal modulation represents another significant benefit of EECP therapy. The treatment helps normalize sympathetic nervous system activity and reduces levels of stress hormones that contribute to disease progression. These changes promote myocardial recovery and prevent further deterioration.
Improved ventricular function occurs through multiple mechanisms including enhanced preload, reduced afterload, and improved coronary perfusion. EECP therapy has been shown to significantly increase LVEF and significantly reduce resting heart rate. These improvements translate into better exercise tolerance and quality of life for patients.
EECP Treatment Protocol and Administration
Standard EECP treatment protocols have been refined through decades of clinical experience and research. Patients usually undergo 35 consecutive 1-hour sessions of EECP over 5–7 weeks. This intensive schedule allows for cumulative benefits while ensuring patient safety and comfort.
Treatment Sessions
Each EECP session involves careful patient monitoring and cuff pressure optimization. Patients lie comfortably on a treatment bed while pneumatic cuffs are applied to their calves, lower thighs, and upper thighs. ECG monitoring ensures precise synchronization with the cardiac cycle.
Session parameters are individualized based on patient tolerance and hemodynamic response. Pressure levels typically range from 200-300 mmHg, adjusted according to patient comfort and therapeutic goals. Continuous monitoring allows for real-time adjustments to optimize treatment effectiveness.
Treatment Response Monitoring
Regular assessment during EECP therapy helps track patient progress and adjust treatment parameters. Symptom improvement, exercise tolerance, and quality of life measures provide valuable feedback about treatment effectiveness. Objective measures such as echocardiography may be performed to assess cardiac function changes.
Patient education plays a crucial role in treatment success. Understanding the therapy mechanism and expected timeline for improvement helps patients remain committed to the treatment schedule. Support from healthcare teams enhances compliance and treatment outcomes.
Clinical Evidence Supporting EECP in Heart Failure
Extensive research demonstrates EECP’s effectiveness in treating various forms of heart failure, including dilated cardiomyopathy. According to existing evidence, the standard course of EECP is safe in patients with IHF and can significantly improve the quality of life of these patients. This safety profile makes it an attractive option for patients who may not be candidates for more invasive procedures.
Research Findings
Clinical studies consistently show improvements in functional capacity and symptom burden following EECP therapy. Most patients demonstrated a significant decrease in angina and improvement in quality of life after EECP and this decrease was maintained in most patients at 2-year follow-up. These sustained benefits indicate that EECP provides lasting therapeutic effects rather than temporary symptom relief.
Objective measures of cardiac function also show improvement with EECP therapy. Studies report enhanced left ventricular ejection fraction, improved exercise tolerance, and reduced hospitalizations. These outcomes translate into meaningful clinical benefits for patients with dilated cardiomyopathy.
Long-term Outcomes
Follow-up studies demonstrate durability of EECP benefits extending well beyond the treatment period. Patients maintain improved functional status and quality of life measures for years after completing therapy. This sustained benefit profile supports EECP as a valuable long-term treatment strategy.
Reduced healthcare utilization represents an important secondary benefit of EECP therapy. Patients experience fewer hospitalizations, emergency department visits, and need for additional cardiac procedures. These outcomes provide both clinical and economic advantages.
EECP vs. Alternative Treatments: Comprehensive Comparison
| Treatment Parameter | EECP Therapy | Medication Therapy | Surgical Intervention | Device Therapy |
|---|---|---|---|---|
| Invasiveness | Non-invasive | Non-invasive | Highly invasive | Moderately invasive |
| Hospital Stay | Outpatient | Outpatient | 5-14 days | 2-5 days |
| Recovery Time | Immediate | Immediate | 6-12 weeks | 2-4 weeks |
| Success Rate | 70-85% | 60-75% | 80-90% | 75-85% |
| Complication Risk | <1% | 15-25% | 10-20% | 5-15% |
| Long-term Benefits | 2-5 years | Ongoing | 10-15 years | 5-10 years |
| Cost Effectiveness | High | Moderate | Low | Moderate |
| Patient Comfort | High | Variable | Low | Moderate |
| Repeat Treatments | Possible | Ongoing | Limited | Possible |
Advantages of EECP Therapy
EECP therapy offers unique advantages over traditional treatments for dilated cardiomyopathy. The non-invasive nature eliminates surgical risks while providing meaningful clinical benefits. Patients can continue normal activities throughout treatment, maintaining their quality of life during the therapeutic process.
Cost-effectiveness analysis favors EECP therapy for many patients with dilated cardiomyopathy. The absence of hospitalization costs, surgical fees, and complication management expenses makes EECP an economically attractive option. Insurance coverage for EECP continues to expand as evidence supports its effectiveness.
Treatment Combinations
EECP therapy complements rather than replaces other cardiac treatments. Patients can continue their medications while receiving EECP, potentially enhancing overall therapeutic effectiveness. This compatibility allows for comprehensive treatment approaches tailored to individual patient needs.
Sequential treatment strategies may involve EECP as initial therapy, with more invasive options reserved for non-responders. This approach minimizes patient risk while maximizing therapeutic benefit. Treatment algorithms incorporating EECP help optimize resource utilization and patient outcomes.
Who Needs EECP Treatment for Dilated Cardiomyopathy?
EECP therapy benefits specific patient populations with dilated cardiomyopathy who meet certain clinical criteria. Understanding these indications helps identify appropriate candidates for this innovative treatment approach.
Primary Candidates
Patients with symptomatic dilated cardiomyopathy experiencing exercise intolerance or chest discomfort represent ideal EECP candidates. Those who have not achieved optimal symptom control with maximum medical therapy may benefit significantly from EECP treatment. Functional limitations that impact quality of life serve as strong indications for EECP consideration.
Individuals seeking non-invasive treatment alternatives find EECP particularly attractive. Patients who are poor surgical candidates due to age, comorbidities, or personal preference can achieve meaningful clinical improvement through EECP therapy. Risk-averse patients appreciate the excellent safety profile of this treatment modality.
Clinical Indications
Heart failure symptoms including dyspnea, fatigue, and exercise intolerance provide clear indications for EECP therapy. Patients with New York Heart Association Class II-III symptoms typically experience the most dramatic improvements. Objective measures such as reduced ejection fraction support EECP candidacy.
Refractory angina in patients with dilated cardiomyopathy represents a specific indication for EECP therapy. EECP therapy has been shown to be beneficial for reducing shortness of breath in patients with heart disease. These symptom improvements translate into enhanced quality of life and functional capacity.
Patient Selection Criteria
Comprehensive evaluation ensures appropriate patient selection for EECP therapy. Cardiac catheterization results, echocardiographic findings, and stress testing help determine candidacy. Patients with preserved peripheral circulation and absence of significant aortic insufficiency represent optimal candidates.
Contraindications for EECP therapy are relatively few but important to recognize. Severe peripheral vascular disease, active bleeding disorders, and certain arrhythmias may preclude EECP treatment. Careful screening ensures patient safety and treatment effectiveness.
Benefits and Mechanisms of EECP in Cardiac Recovery
EECP therapy provides multiple therapeutic benefits that address the complex pathophysiology of dilated cardiomyopathy. These mechanisms work synergistically to promote cardiac recovery and improve patient outcomes.
Hemodynamic Improvements
Enhanced coronary perfusion represents the primary mechanism through which EECP benefits patients with dilated cardiomyopathy. Increased diastolic pressure augmentation improves oxygen delivery to compromised myocardium. This enhanced perfusion supports cellular recovery and prevents further ischemic damage.
Afterload reduction allows the weakened heart to pump more efficiently, reducing energy consumption and improving cardiac output. This hemodynamic unloading provides immediate symptom relief while promoting long-term cardiac recovery. The combination of enhanced perfusion and reduced workload creates optimal conditions for myocardial healing.
Cellular and Molecular Effects
EECP therapy stimulates multiple cellular pathways that promote cardiac recovery. Enhanced shear stress activates endothelial cells, promoting nitric oxide production and vasodilation. Growth factor release supports angiogenesis and tissue repair processes.
Neurohormonal modulation through EECP therapy helps normalize the pathological changes associated with dilated cardiomyopathy. Reduced sympathetic nervous system activation and improved baroreceptor sensitivity contribute to hemodynamic stability. These changes support long-term cardiac recovery beyond the immediate treatment effects.
Functional Improvements
Exercise tolerance improvements represent one of the most significant benefits of EECP therapy for patients with dilated cardiomyopathy. Enhanced cardiac output and improved oxygen delivery translate into better physical performance. Patients report increased ability to perform daily activities and reduced fatigue levels.
Quality of life improvements encompass physical, emotional, and social domains. Reduced symptoms allow patients to resume activities they previously avoided. Improved sleep quality, reduced anxiety, and enhanced social interactions contribute to overall well-being.
Safety Profile and Contraindications
EECP therapy demonstrates an excellent safety profile with minimal adverse effects reported in clinical studies. This safety record makes it an attractive option for patients who may be at high risk for complications with other treatments.
Safety Data
Clinical trials consistently report low complication rates with EECP therapy. Minor side effects such as skin irritation or leg discomfort occur in less than 5% of patients and typically resolve with treatment modifications. Serious adverse events are extremely rare, occurring in less than 0.1% of patients.
Long-term safety data support the use of EECP therapy in patients with various cardiac conditions. No evidence of long-term adverse effects has been reported, even with repeated treatment courses. This safety profile supports EECP as a viable long-term treatment strategy.
Contraindications and Precautions
Absolute contraindications for EECP therapy include severe aortic insufficiency, active bleeding disorders, and severe peripheral vascular disease. These conditions may be exacerbated by the hemodynamic changes induced by EECP therapy.
Relative contraindications require careful consideration and may include pregnancy, severe hypertension, and certain arrhythmias. Each patient requires individual assessment to determine the appropriateness of EECP therapy. Risk-benefit analysis guides treatment decisions in borderline cases.
Lifestyle Modifications and Supportive Care
EECP therapy works optimally when combined with comprehensive lifestyle modifications that support cardiac health. These interventions enhance treatment effectiveness and promote long-term wellness.
Nutritional Strategies
Cardiac-specific nutrition plans support the benefits of EECP therapy by addressing underlying metabolic factors that contribute to dilated cardiomyopathy. Sodium restriction helps manage fluid retention and reduces cardiac workload. Anti-inflammatory diets rich in omega-3 fatty acids support myocardial recovery.
Micronutrient optimization ensures adequate levels of vitamins and minerals essential for cardiac function. Magnesium, potassium, and B-vitamins play crucial roles in myocardial metabolism and electrical stability. Nutritional counseling helps patients implement sustainable dietary changes that support cardiac health.
Exercise Rehabilitation
Structured exercise programs complement EECP therapy by promoting cardiovascular fitness and functional capacity. Cardiac rehabilitation protocols adapted for patients with dilated cardiomyopathy provide safe and effective exercise prescriptions. Progressive training programs help patients rebuild strength and endurance.
Exercise timing in relation to EECP treatments may influence outcomes. Some patients benefit from light exercise following EECP sessions, while others require rest periods. Individualized exercise prescriptions optimize the synergistic effects of EECP and physical activity.
Stress Management
Psychological stress contributes to the progression of dilated cardiomyopathy through neurohormonal activation and lifestyle factors. Stress reduction techniques such as meditation, yoga, and counseling support the benefits of EECP therapy. Mind-body interventions help patients develop coping strategies for managing chronic illness.
Sleep optimization represents another important aspect of supportive care. Quality sleep supports cardiac recovery and enhances the benefits of EECP therapy. Sleep hygiene education and treatment of sleep disorders contribute to overall treatment success.
Future Directions and Research
Ongoing research continues to expand our understanding of EECP therapy’s mechanisms and optimal applications. Future developments promise to enhance treatment effectiveness and broaden patient populations who can benefit from this innovative therapy.
Emerging Technologies
Advanced monitoring technologies may allow for more precise EECP treatment optimization. Real-time hemodynamic monitoring could guide pressure adjustments and treatment modifications. Artificial intelligence applications might help predict treatment response and optimize protocols.
Combination therapies incorporating EECP with other innovative treatments show promise for enhanced outcomes. Stem cell therapy, gene therapy, and novel pharmacological agents may work synergistically with EECP to promote cardiac regeneration. These multimodal approaches represent the future of cardiac care.
Research Opportunities
Long-term studies tracking EECP benefits over decades will provide valuable insights into treatment durability. Genetic studies may identify patient populations most likely to benefit from EECP therapy. Biomarker research could help predict treatment response and optimize patient selection.
International collaborations are expanding EECP research to diverse patient populations and healthcare systems. These studies will help establish global treatment protocols and identify cultural factors that influence treatment outcomes. Evidence-based guidelines will continue to evolve as research expands.
Conclusion: Transforming Cardiac Care Through EECP
EECP treatment for dilated cardiomyopathy represents a paradigm shift toward non-invasive, patient-centered cardiac care. This innovative therapy addresses the complex pathophysiology of dilated cardiomyopathy while minimizing treatment risks and maximizing patient comfort.
The compelling clinical evidence supporting EECP therapy continues to grow, with studies demonstrating sustained improvements in symptoms, functional capacity, and quality of life. As healthcare systems worldwide seek cost-effective treatments that provide meaningful patient benefits, EECP emerges as an optimal solution for many patients with dilated cardiomyopathy.
Patients facing the challenges of dilated cardiomyopathy now have access to a proven, safe, and effective treatment option that complements traditional therapies. EECP therapy offers hope for improved outcomes without the risks associated with invasive procedures. As research continues to refine treatment protocols and expand applications, EECP will likely play an increasingly important role in comprehensive cardiac care.
The future of dilated cardiomyopathy treatment lies in personalized, multimodal approaches that address individual patient needs and preferences. EECP therapy, with its excellent safety profile and proven effectiveness, represents a cornerstone of this evolving treatment landscape. Patients and healthcare providers can confidently consider EECP as a valuable component of comprehensive cardiac care plans.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As an expert in treating patients with lifestyle disorders, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar serves as the Founder of FIT MY HEART and works as a Consultant at NEXIN HEALTH and MD CITY Hospital Noida. His extensive experience in cardiovascular care and innovative non-surgical treatment approaches makes him a leading authority in integrated EECP therapy applications combined with holistic healing methods.
His practice focuses on providing comprehensive alternatives to traditional cardiac interventions, helping patients achieve optimal cardiovascular health through evidence-based non-surgical treatments combined with lifestyle optimization and natural healing approaches.
For more information about integrated non-surgical cardiac treatments and comprehensive cardiovascular health services, visit www.viveksengar.in.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurverdic Heart Blockage Treatment
Revolutionary Non Surgical Heart Treatment
Frequently Asked Questions: EECP Treatment for Dilated Cardiomyopathy
Que: What is EECP treatment in Dilated Cardiomyopathy (DCM)?
Ans: EECP (Enhanced External Counter Pulsation) is a non-invasive therapy that improves blood flow to the heart, helping DCM patients manage symptoms without surgery.
Que: How does EECP help in Dilated Cardiomyopathy?
Ans: EECP improves collateral circulation, enhances oxygen delivery to weak heart muscles, and supports better cardiac output in DCM patients.
Que: Is EECP a permanent solution for DCM?
Ans: EECP is not a cure, but it offers long-term symptom relief and improved quality of life when combined with lifestyle changes.
Que: How many sessions of EECP are required for DCM treatment?
Ans: Typically, 35 to 40 sessions (1 hour each) over 6 weeks are recommended for effective results in DCM patients.
Que: Is EECP treatment painful?
Ans: No, EECP is a painless, safe, and FDA-approved therapy for heart conditions including DCM.
Que: Can EECP improve ejection fraction (LVEF) in DCM patients?
Ans: Yes, studies and clinical experience show that EECP can gradually improve LVEF in many DCM patients.
Que: Who is eligible for EECP treatment in DCM?
Ans: Patients with stable Dilated Cardiomyopathy, low LVEF, fatigue, breathlessness, or heart failure symptoms may be eligible after evaluation.
Que: Are there any side effects of EECP therapy?
Ans: EECP is generally safe with minimal side effects like muscle soreness or mild skin irritation, which are temporary.
Que: Can EECP reduce the need for heart transplant in DCM?
Ans: In many cases, EECP improves heart function enough to delay or avoid the need for transplant or surgical intervention.
Que: Is EECP covered under insurance or health plans?
Ans: In many countries, EECP is covered under insurance for specific cardiac indications, but coverage depends on the provider.
Que: How long do the benefits of EECP last in DCM patients?
Ans: Benefits can last for several months to years, especially with proper diet, exercise, and medical follow-up.
Que: Can EECP be repeated if symptoms return?
Ans: Yes, EECP can be safely repeated based on your cardiologist’s advice if symptoms of DCM return.
Que: What are the contraindications of EECP in DCM patients?
Ans: Contraindications include severe aortic regurgitation, active deep vein thrombosis, or uncontrolled hypertension.
Que: Is EECP effective in end-stage Dilated Cardiomyopathy?
Ans: EECP may provide symptom relief in advanced stages, but effectiveness depends on individual health status and should be medically assessed.
Que: Where can I get EECP treatment for Dilated Cardiomyopathy?
Ans: EECP is available at specialized cardiac and non-invasive therapy centers; consult a certified EECP practitioner or cardiologist near you.
References
- Enhanced External Counterpulsation in Ischemic Heart Failure: A Systematic Review. Current Cardiology Reports, 2023.
- The Role of Enhanced External Counter Pulsation Therapy in Clinical Practice. PMC, 2014.
- Two-Year Clinical Outcomes After Enhanced External Counterpulsation (EECP) Therapy in Patients With Refractory Angina Pectoris and Left Ventricular Dysfunction. American Journal of Cardiology, 2005.
- Dilated Cardiomyopathy. Nature Reviews Disease Primers, 2019.
- Fifteen-year mortality and prognostic factors in patients with dilated cardiomyopathy. PMC, 2022.
- Prevalence of Genetically Associated Dilated Cardiomyopathy: A Systematic Literature Review and Meta-Analysis. Cardiology Research, 2023.
- 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation, 2024.
- Epidemiology – Dilated Cardiomyopathy. NCBI Bookshelf, 2024.
Note: This blog is for educational purposes only and should not replace professional medical advice. Always consult with qualified healthcare providers before making treatment decisions.