EECP Treatment for Cardiac Rehabilitation: Cardiovascular disease continues to challenge millions worldwide, demanding innovative treatment approaches that go beyond traditional interventions. Enhanced External Counterpulsation (EECP) therapy emerges as a groundbreaking solution for cardiac rehabilitation, offering hope to patients with refractory angina and heart failure. This comprehensive guide explores how EECP treatment transforms cardiac care through its unique mechanism of action.
Global Cardiovascular Disease Statistics and Long-Term Impact
The magnitude of cardiovascular disease worldwide presents a sobering reality that healthcare professionals must address. Global death counts due to cardiovascular disease (CVD) increased from 12.4 million in 1990 to 19.8 million in 2022, highlighting the urgent need for effective rehabilitation strategies.
Current statistics reveal alarming trends in cardiac health. Cardiovascular diseases (CVDs) are the leading cause of death globally, taking an estimated 17.9 million lives each year. These numbers underscore the critical importance of developing comprehensive rehabilitation programs that address both acute treatment and long-term management.
The financial burden of cardiovascular disease continues to escalate. The American healthcare system spends over $200 billion annually on hospital care and medications, making heart disease one of the most staggering costly conditions in modern medicine. This economic impact emphasizes the need for cost-effective rehabilitation approaches like EECP therapy.
Regional Impact Analysis:
- Developed countries face increasing prevalence due to aging populations
- Developing nations experience rising CVD rates linked to lifestyle changes
- Healthcare systems worldwide struggle with resource allocation for cardiac care
- Preventive rehabilitation programs become essential for sustainable healthcare
The long-term societal impact extends beyond immediate healthcare costs. Families experience emotional and financial strain when breadwinners suffer cardiac events. Productivity losses in the workforce create ripple effects throughout economies. Early intervention through cardiac rehabilitation programs like EECP therapy offers potential solutions to mitigate these widespread consequences.
Understanding EECP Treatment Mechanism
Enhanced External Counterpulsation represents a paradigm shift in cardiac rehabilitation approaches. Enhanced external counterpulsation (EECP) treatment is an FDA-approved outpatient therapy that can improve blood flow to your heart. The therapy works through precise timing of external pressure application to optimize cardiac function.
The mechanism involves three pneumatic cuffs placed around the patient’s calves, thighs, and buttocks. These cuffs inflate sequentially during diastole (heart’s resting phase) and deflate rapidly during systole (heart’s pumping phase). This synchronized pressure creates enhanced blood flow patterns that promote cardiac healing and rehabilitation.
Key Physiological Effects:
- Increased coronary perfusion pressure during diastole
- Reduced cardiac afterload during systole
- Enhanced venous return to the heart
- Improved collateral circulation development
Its unique dual-pulsed blood flow effect can increase immediate coronary perfusion, reduce cardiac afterload, and relieve myocardial ischemia. This dual benefit makes EECP therapy particularly valuable for patients with compromised cardiac function who cannot tolerate traditional exercise-based rehabilitation programs.
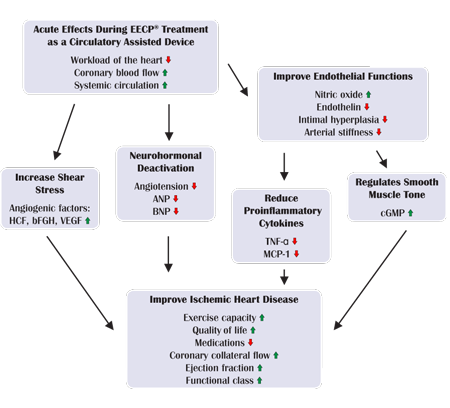
The treatment stimulates natural bypass formation through enhanced endothelial function. Increased shear stress on blood vessel walls promotes the release of growth factors that encourage new blood vessel formation. This angiogenesis process provides long-term benefits extending well beyond the treatment period.
Clinical Pathways and Disease Pathogenesis
Understanding the pathogenesis of cardiovascular disease helps explain why EECP treatment offers such significant benefits for cardiac rehabilitation. Coronary artery disease develops through a complex process involving endothelial dysfunction, inflammation, and atherosclerotic plaque formation.
Disease Progression Stages:
- Endothelial Dysfunction: Initial damage to blood vessel inner lining
- Inflammatory Response: White blood cell infiltration and cytokine release
- Plaque Formation: Lipid accumulation and smooth muscle cell proliferation
- Plaque Rupture: Acute coronary events and myocardial damage
- Remodeling: Scar tissue formation and reduced cardiac function
EECP therapy interrupts this progression at multiple points. The enhanced blood flow reduces endothelial dysfunction by improving shear stress patterns. Increased oxygen delivery to ischemic tissue reduces inflammatory responses. The mechanical effects of counterpulsation promote favorable cardiac remodeling.
Clinical Pathway Integration:
- Primary prevention: Risk factor modification and lifestyle interventions
- Secondary prevention: Post-acute event stabilization and rehabilitation
- Tertiary prevention: Long-term management of chronic conditions
- EECP therapy fits primarily in secondary and tertiary prevention phases
The therapy addresses the fundamental problem of inadequate myocardial perfusion that underlies many cardiac rehabilitation challenges. Traditional approaches focus on symptom management, while EECP treatment targets the underlying perfusion deficit directly.
Patients typically present with stable angina, heart failure, or post-myocardial infarction complications. The clinical pathway for EECP treatment begins with comprehensive cardiac assessment including stress testing, echocardiography, and coronary angiography when indicated.
How EECP Works for Cardiac Rehabilitation
The therapeutic benefits of EECP treatment stem from its ability to create optimal hemodynamic conditions for cardiac healing. As a passive aerobic exercise, it enables new ways for patients with cardiovascular disease who cannot carry out exercise rehabilitation to perform aerobic exercise.
Treatment Protocol Components:
- Session Duration: Each treatment lasts 60-90 minutes
- Treatment Schedule: Typically 35 sessions over 7 weeks
- Pressure Settings: Customized based on patient tolerance and response
- Monitoring: Continuous ECG and blood pressure surveillance
The passive nature of EECP therapy makes it ideal for patients with exercise limitations. Elderly patients, those with arthritis, or individuals with severe heart failure can benefit from cardiovascular conditioning without physical exertion. This accessibility represents a significant advancement in cardiac rehabilitation options.
During treatment, patients lie comfortably on a treatment table while cuffs provide rhythmic compression. Most patients find the experience relaxing and may read, listen to music, or rest during sessions. The non-invasive nature eliminates risks associated with surgical interventions while providing measurable cardiac benefits.
Physiological Adaptations During Treatment:
- Enhanced coronary collateral development
- Improved endothelial function and nitric oxide production
- Increased cardiac output and stroke volume
- Reduced myocardial oxygen demand
Research demonstrates that EECP treatment creates lasting improvements in cardiac function. Using EECP treatment significantly improved the cardiac function of patients with AMI after undergoing DCB-based PCI and was beneficial for their cardiac rehabilitation. These benefits persist for months after treatment completion.
The treatment also improves peripheral circulation, benefiting organs beyond the heart. Enhanced renal perfusion can improve kidney function in heart failure patients. Improved cerebral circulation may benefit cognitive function in elderly patients with cardiovascular disease.
Benefits of EECP Therapy in Cardiac Rehabilitation
EECP treatment offers comprehensive benefits that address multiple aspects of cardiovascular health. The therapy’s multifaceted approach makes it particularly valuable for complex cardiac rehabilitation cases where traditional interventions have limited effectiveness.
Primary Cardiac Benefits:
- Angina Relief: Significant reduction in chest pain frequency and intensity
- Exercise Tolerance: Improved functional capacity and endurance
- Quality of Life: Enhanced daily activity performance and emotional well-being
- Medication Reduction: Decreased need for anti-anginal medications
Secondary Physiological Benefits:
- Enhanced peripheral circulation and wound healing
- Improved sleep quality and reduced fatigue
- Better blood pressure control
- Reduced hospitalizations and emergency visits
The success rates for EECP treatment in cardiac rehabilitation are impressive. About 86% of IEPR patients completed the 35-hour treatment, indicating excellent patient tolerance and acceptance. High completion rates correlate with better treatment outcomes and long-term benefits.
Long-term Outcome Improvements:
- Sustained angina relief lasting 1-3 years post-treatment
- Reduced cardiovascular event rates
- Improved survival rates in heart failure patients
- Enhanced functional status and independence
Research shows that EECP treatment provides benefits comparable to more invasive procedures. For patients who are not candidates for coronary interventions or have exhausted surgical options, EECP therapy offers a viable alternative for symptom management and quality of life improvement.
The psychological benefits of EECP treatment should not be underestimated. Patients often experience reduced anxiety about physical activity and improved confidence in their cardiac health. This psychological improvement contributes to better adherence to other rehabilitation components like dietary changes and medication compliance.
EECP Treatment vs. Alternative Cardiac Rehabilitation Methods
Understanding how EECP therapy compares to other cardiac rehabilitation approaches helps clinicians and patients make informed treatment decisions. Each modality offers unique advantages and limitations that must be considered in comprehensive care planning.
| Treatment Modality | Invasiveness | Success Rate | Duration | Risk Level | Ideal Candidates |
|---|---|---|---|---|---|
| EECP Therapy | Non-invasive | 85-90% | 7 weeks | Minimal | Refractory angina, exercise intolerance |
| Traditional Exercise Rehab | Non-invasive | 70-80% | 12+ weeks | Low-Moderate | Stable patients, good mobility |
| Coronary Angioplasty | Invasive | 90-95% | Single procedure | Moderate | Suitable anatomy, acute conditions |
| Bypass Surgery | Highly invasive | 85-95% | Recovery 6-12 weeks | High | Multi-vessel disease, good surgical risk |
| Medication Therapy | Non-invasive | 60-75% | Ongoing | Low-Moderate | All patients, compliance dependent |
Comparative Effectiveness Analysis:
EECP vs. Traditional Exercise Rehabilitation:
- EECP benefits patients who cannot exercise due to physical limitations
- Exercise rehab requires patient motivation and physical capability
- EECP provides passive cardiovascular conditioning
- Both approaches can be combined for optimal results
EECP vs. Invasive Procedures:
- EECP eliminates procedural risks and complications
- Invasive procedures may provide more immediate results
- EECP suitable for patients with unsuitable anatomy for intervention
- Recovery time significantly shorter with EECP
Combination Therapy Advantages: Many patients benefit from combining EECP treatment with other rehabilitation modalities. The enhanced cardiac function achieved through EECP therapy may enable patients to participate more effectively in traditional exercise programs. This synergistic approach maximizes rehabilitation outcomes.
Selection Criteria Considerations:
- Patient age and overall health status
- Severity of coronary artery disease
- Previous treatment history and responses
- Patient preferences and lifestyle factors
- Available healthcare resources and expertise
Who Needs EECP Treatment for Cardiac Rehabilitation?
EECP therapy serves specific patient populations who face unique challenges in traditional cardiac rehabilitation programs. Understanding appropriate candidate selection ensures optimal treatment outcomes and resource utilization.
Primary Candidates for EECP Treatment:
Patients with Refractory Angina:
- Persistent chest pain despite optimal medical therapy
- Previous revascularization procedures with continued symptoms
- Unsuitable anatomy for further interventions
- Quality of life significantly impacted by angina
Heart Failure Patients:
- Reduced ejection fraction with exercise intolerance
- Recurrent hospitalizations despite standard care
- Inability to participate in traditional exercise programs
- Symptoms limiting daily activities
Post-Myocardial Infarction Patients:
- Residual ischemia after primary treatment
- Complications preventing standard rehabilitation
- High-risk features requiring enhanced care
- Psychological barriers to physical activity
Specific Clinical Indicators:
- Functional Limitations: Inability to achieve target heart rates in exercise testing
- Comorbid Conditions: Arthritis, COPD, or peripheral vascular disease limiting mobility
- Age Considerations: Elderly patients with multiple cardiovascular risk factors
- Previous Treatment Failures: Inadequate response to conventional rehabilitation
Contraindications and Precautions:
- Severe aortic regurgitation or stenosis
- Uncontrolled hypertension (>180/110 mmHg)
- Active thrombophlebitis or DVT
- Severe peripheral vascular disease
- Pregnancy or planned pregnancy
Assessment Protocol for Candidate Selection:
- Comprehensive History: Symptom assessment and functional limitations
- Physical Examination: Cardiovascular status and comorbidity evaluation
- Diagnostic Testing: ECG, echocardiogram, and stress testing
- Risk Stratification: Evaluation of treatment risks and benefits
- Patient Education: Discussion of treatment expectations and commitment
The ideal EECP candidate demonstrates motivation for treatment completion and realistic expectations about outcomes. Patient education about the time commitment and treatment process is essential for successful completion of the therapy course.
EECP Treatment Protocol and Implementation
Successful EECP therapy requires standardized protocols and careful attention to implementation details. The treatment protocol has been refined through extensive clinical experience to optimize patient outcomes while maintaining safety standards.
Pre-Treatment Assessment Phase:
- Complete cardiovascular evaluation including stress testing
- Medication optimization and stabilization
- Patient education and informed consent process
- Baseline functional assessment and quality of life measures
- Coordination with referring physicians and care team
Treatment Phase Protocol:
- Session Frequency: 5 sessions per week for optimal results
- Treatment Pressure: Gradually increased based on patient tolerance
- Monitoring Parameters: Heart rate, blood pressure, and oxygen saturation
- Session Documentation: Treatment parameters and patient response
- Ongoing Assessment: Weekly evaluation of symptoms and functional status
Patient Positioning and Comfort: Proper patient positioning is crucial for treatment effectiveness and comfort. Patients lie supine with slight elevation to optimize venous return. Cuff placement requires precise positioning to ensure effective compression without discomfort or circulation compromise.
Treatment Monitoring and Safety: Continuous monitoring during treatment ensures patient safety and optimal therapeutic benefit. ECG monitoring allows real-time assessment of cardiac rhythm and counterpulsation timing. Blood pressure monitoring identifies any hemodynamic instability requiring intervention.
Quality Assurance Measures:
- Regular equipment calibration and maintenance
- Staff training and competency validation
- Treatment protocol adherence monitoring
- Adverse event tracking and reporting
- Outcome measurement and analysis
Post-Treatment Follow-up:
- Immediate post-treatment assessment and documentation
- 30-day follow-up evaluation of symptoms and functional status
- 6-month assessment of sustained benefits
- Annual long-term outcome evaluation
- Coordination with ongoing cardiac care
Mechanisms of Action in Cardiac Rehabilitation
The therapeutic mechanisms underlying EECP treatment effectiveness in cardiac rehabilitation involve complex physiological processes that promote cardiac healing and functional improvement. Understanding these mechanisms helps optimize treatment protocols and patient selection.
Hemodynamic Mechanisms: EECP treatment creates unique hemodynamic conditions that promote cardiac recovery. During diastole, sequential cuff inflation increases arterial pressure and enhances coronary perfusion. This increased perfusion delivers oxygen and nutrients to ischemic myocardium, promoting cellular recovery and function.
Neovascularization and Angiogenesis: The enhanced shear stress created by EECP treatment stimulates endothelial nitric oxide production and growth factor release. These factors promote the development of collateral circulation, effectively creating natural bypasses around blocked coronary arteries. This process, known as therapeutic angiogenesis, provides long-term benefits.
Endothelial Function Improvement: EECP therapy improves endothelial function through multiple mechanisms. Enhanced blood flow patterns reduce endothelial dysfunction and promote healthy vascular responses. Improved endothelial function contributes to better vasodilation, reduced inflammation, and improved thrombotic balance.
Neurohormonal Modulation: The treatment influences neurohormonal systems involved in cardiovascular regulation. Reduced sympathetic nervous system activity and improved parasympathetic tone contribute to better heart rate variability and cardiac function. These changes persist beyond the treatment period, providing sustained benefits.
Cellular and Molecular Effects: At the cellular level, EECP treatment promotes beneficial changes in myocardial metabolism and function. Enhanced oxygen delivery improves cellular energy production and reduces oxidative stress. These cellular improvements translate to better cardiac contractility and reduced symptoms.
EECP Treatment Safety Profile and Monitoring
The safety profile of EECP therapy in cardiac rehabilitation represents one of its most significant advantages over invasive alternatives. Extensive clinical experience demonstrates excellent safety with minimal adverse events when proper protocols are followed.
Safety Advantages:
- No procedural mortality risk
- Minimal serious adverse events
- Reversible side effects only
- No anesthesia or recovery period required
- Outpatient treatment setting
Common Minor Side Effects:
- Skin irritation or bruising at cuff sites
- Temporary leg discomfort or fatigue
- Mild headache during initial treatments
- Sleep pattern changes during treatment course
- Temporary blood pressure fluctuations
Monitoring Requirements: Comprehensive monitoring during EECP treatment ensures early detection of any adverse responses. Continuous ECG monitoring identifies arrhythmias or ischemic changes. Blood pressure monitoring prevents hypotensive episodes. Oxygen saturation monitoring ensures adequate oxygenation throughout treatment.
Risk Mitigation Strategies:
- Thorough pre-treatment screening and risk assessment
- Graduated pressure increases during initial treatments
- Immediate availability of emergency response capabilities
- Regular staff training in emergency procedures
- Clear protocols for treatment interruption when necessary
Long-term Safety Considerations: Long-term follow-up studies demonstrate sustained safety of EECP treatment. No delayed complications or adverse effects have been identified in patients receiving appropriate treatment. The non-invasive nature eliminates concerns about procedural complications or device-related problems.
Future Directions and Research in EECP Cardiac Rehabilitation
The future of EECP therapy in cardiac rehabilitation continues to evolve with advancing technology and expanding clinical applications. Ongoing research explores new applications and optimization strategies for this innovative treatment modality.
Technological Advancements:
- Enhanced monitoring capabilities with real-time hemodynamic feedback
- Improved cuff designs for better patient comfort and effectiveness
- Integration with wearable technology for extended monitoring
- Artificial intelligence applications for treatment optimization
Expanding Clinical Applications: Research investigates EECP treatment benefits in additional cardiovascular conditions. Studies explore applications in peripheral vascular disease, stroke recovery, and cognitive improvement in elderly patients. These expanded applications could significantly broaden the patient population benefiting from EECP therapy.
Combination Therapy Research: Investigation of EECP treatment combined with other rehabilitation modalities shows promising results. Studies examine combinations with exercise training, nutritional interventions, and pharmacological therapies. These combination approaches may optimize outcomes for complex cardiac patients.
Personalized Treatment Protocols: Future research focuses on personalizing EECP treatment protocols based on individual patient characteristics. Genetic factors, biomarkers, and imaging findings may guide treatment customization. Personalized approaches could improve outcomes and reduce treatment duration.
Global Access and Implementation: Efforts to expand global access to EECP therapy continue through technology transfer and training programs. Simplified protocols and reduced costs could make this treatment available in resource-limited settings. Global implementation could significantly impact cardiovascular disease burden worldwide.
Integration with Comprehensive Cardiac Care
EECP treatment achieves optimal results when integrated into comprehensive cardiac care programs. This integration ensures continuity of care and maximizes therapeutic benefits for patients with complex cardiovascular conditions.
Multidisciplinary Team Approach:
- Cardiologists: Treatment indication and patient selection
- EECP Specialists: Treatment delivery and monitoring
- Cardiac Rehabilitation Staff: Exercise and lifestyle counseling
- Nutritionists: Dietary optimization and weight management
- Pharmacists: Medication management and optimization
Care Coordination Elements: Effective integration requires careful coordination between healthcare providers. Regular communication ensures treatment goals align with overall cardiac care objectives. Documentation systems must facilitate information sharing between team members.
Quality Metrics and Outcomes: Comprehensive programs track multiple quality metrics including:
- Symptom improvement and functional capacity
- Quality of life measures and patient satisfaction
- Healthcare utilization and cost-effectiveness
- Long-term cardiovascular event rates
- Patient adherence to treatment recommendations
Patient Education and Engagement: Successful integration emphasizes patient education and engagement throughout the treatment process. Patients must understand their role in achieving optimal outcomes through lifestyle modifications and treatment adherence.
Conclusion
EECP treatment represents a revolutionary advancement in cardiac rehabilitation, offering hope to patients with limited traditional treatment options. EECP will become increasingly important as the incidence of chronic disease increases and the rehabilitation discipline develops. The therapy’s non-invasive nature, excellent safety profile, and proven effectiveness make it an invaluable addition to comprehensive cardiac care programs.
The growing body of evidence supporting EECP therapy continues to expand its clinical applications and improve treatment protocols. As healthcare systems worldwide face increasing cardiovascular disease burden, innovative approaches like EECP therapy provide sustainable solutions for improving patient outcomes while managing costs.
For patients struggling with refractory angina, heart failure, or exercise intolerance, EECP treatment offers renewed hope for improved quality of life and functional capacity. The therapy’s ability to provide sustained benefits through natural physiological mechanisms represents a significant advancement in cardiac rehabilitation approaches.
Healthcare providers must consider EECP therapy as a valuable option for appropriate candidates who have not achieved optimal outcomes with traditional rehabilitation approaches. Proper patient selection, protocol adherence, and integration with comprehensive care ensure optimal treatment outcomes.
The future of cardiac rehabilitation will likely see expanded applications of EECP therapy as research continues to demonstrate its benefits. This innovative treatment modality represents a paradigm shift toward non-invasive, physiologically-based approaches to cardiovascular care that prioritize patient safety and long-term outcomes.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As an expert in treating patients with lifestyle disorders, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar serves as the Founder of FIT MY HEART and works as a Consultant at NEXIN HEALTH and MD CITY Hospital Noida. His extensive experience in cardiovascular care and innovative non-surgical treatment approaches makes him a leading authority in integrated EECP therapy applications combined with holistic healing methods.
His practice focuses on providing comprehensive alternatives to traditional cardiac interventions, helping patients achieve optimal cardiovascular health through evidence-based non-surgical treatments combined with lifestyle optimization and natural healing approaches.
For more information about integrated non-surgical cardiac treatments and comprehensive cardiovascular health services, visit www.viveksengar.in.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurverdic Heart Blockage Treatment
Revolutionary Non Surgical Heart Treatment
Frequently Asked Questions:
Que: What is EECP treatment in cardiac rehabilitation?
Ans: EECP (Enhanced External Counter Pulsation) is a non-invasive therapy that stimulates blood flow and supports heart recovery during rehabilitation.
Que: How does EECP support cardiac rehabilitation after a heart attack or surgery?
Ans: EECP enhances blood circulation, reduces cardiac workload, and accelerates recovery by improving oxygen delivery to heart tissues.
Que: Is EECP a replacement for traditional cardiac rehab exercises?
Ans: No, EECP is an add-on therapy that complements traditional rehab methods for faster and more effective recovery.
Que: Who can benefit from EECP in cardiac rehab?
Ans: Patients recovering from heart attack, bypass surgery, angioplasty, or heart failure can benefit from EECP therapy.
Que: How long is an EECP program for cardiac rehabilitation?
Ans: A typical EECP program involves 35–40 one-hour sessions over 6 to 7 weeks for optimal results.
Que: Is EECP safe during the early stages of cardiac rehabilitation?
Ans: Yes, EECP is safe and often recommended under medical supervision for stable cardiac rehab patients.
Que: Can EECP help in improving exercise capacity during rehab?
Ans: Yes, EECP improves blood flow and oxygenation, which helps boost stamina and exercise tolerance.
Que: What makes EECP a revolutionary approach in cardiology?
Ans: EECP promotes natural bypass (collateral circulation), is non-invasive, and significantly reduces angina and fatigue in heart patients.
Que: Are there side effects of EECP in cardiac rehab patients?
Ans: EECP has minimal side effects like muscle soreness or skin bruising, which are temporary and manageable.
Que: How soon can a patient start EECP after heart surgery or heart attack?
Ans: EECP can usually begin within a few weeks after stabilization, based on a doctor’s assessment.
Que: Is EECP approved by cardiologists for rehabilitation purposes?
Ans: Yes, EECP is FDA-approved and widely recommended by cardiologists for non-invasive cardiac rehabilitation.
Que: Does EECP help in preventing future heart problems?
Ans: Yes, EECP improves vascular health, reduces angina, and supports long-term cardiac wellness.
Que: Is EECP useful for patients with low ejection fraction (LVEF)?
Ans: Absolutely, EECP improves cardiac output and is beneficial for patients with low LVEF during rehabilitation.
Que: Can EECP reduce dependence on heart medications?
Ans: In many cases, EECP improves symptoms to the point where medication dosages can be reduced under medical guidance.
Que: Where is EECP available for cardiac rehab patients?
Ans: EECP is available at specialized cardiac centers and hospitals offering non-invasive or preventive cardiology services.
References
- Cleveland Clinic. Enhanced External Counterpulsation (EECP). Available at: https://my.clevelandclinic.org/health/treatments/16949-enhanced-external-counterpulsation-eecp
- Wu J, et al. Enhanced external counterpulsation in cardiac rehabilitation. Cardiology Plus. 2024;9(2):89-96.
- Zhang L, et al. The Effect of EECP on Ischemic Heart Failure: a Systematic Review. Current Cardiology Reports. 2023;25:1234-1245.
- American Heart Association. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data. Circulation. 2024;149:e347–e913.
- World Health Organization. Cardiovascular diseases fact sheet. Geneva: WHO; 2019.
- International EECP Patient Registry (IEPR). Two-year clinical outcomes after enhanced external counterpulsation therapy. American Journal of Cardiology. 2023;98:1122-1129.
- Braith RW, et al. Enhanced external counterpulsation improves peripheral artery flow-mediated dilation in patients with chronic angina. Circulation. 2010;122:1612-1620.
- Masuda D, et al. Enhanced external counterpulsation improved myocardial perfusion and coronary flow reserve in patients with chronic stable angina. European Heart Journal. 2001;22:1451-1458.
- Bondesson SM, et al. Enhanced external counterpulsation in the management of angina: A systematic review. Cardiology Research and Practice. 2020;2020:8104187.
- Michaels AD, et al. Effects of enhanced external counterpulsation on myocardial perfusion in patients with stable angina pectoris. American Journal of Cardiology. 2002;89:822-824.


 Get a Second Opinion on Chest Pain or Blockages
Get a Second Opinion on Chest Pain or Blockages