EECP Treatment for Hypertrophic Cardiomyopathy Management: Hypertrophic cardiomyopathy presents unique challenges in cardiac care, requiring specialized therapeutic approaches that address both symptoms and underlying pathophysiology. Enhanced External Counterpulsation (EECP) emerges as a promising non-invasive treatment option for patients struggling with this complex genetic heart condition.
The conventional management of hypertrophic cardiomyopathy often relies on medications and invasive procedures, but EECP therapy offers a revolutionary alternative. This innovative treatment approach provides hope for patients who experience persistent symptoms despite optimal medical therapy or those unsuitable for surgical interventions.
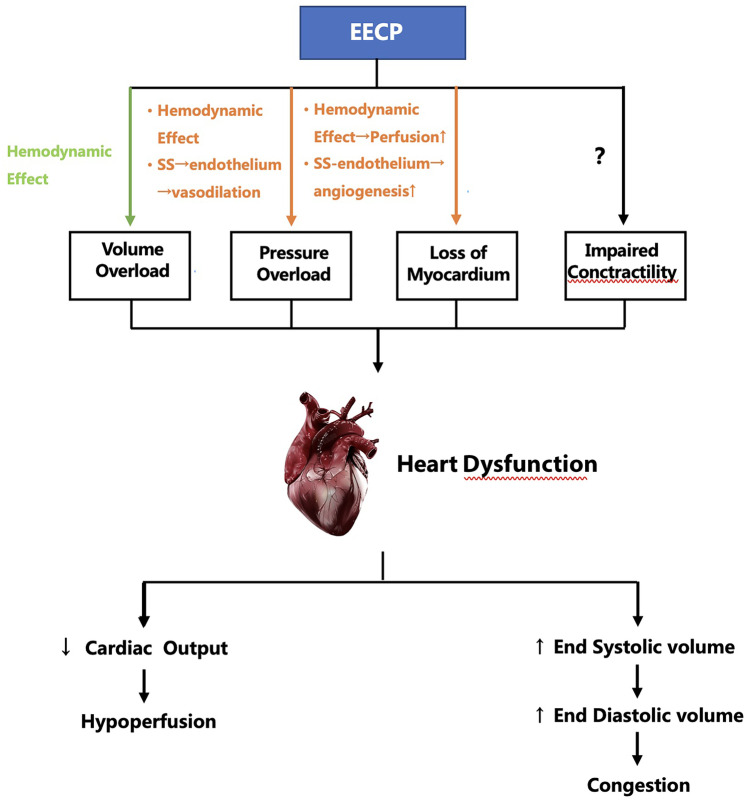
Understanding how EECP therapy works in the context of hypertrophic cardiomyopathy requires examining the unique pathophysiology of this condition. The therapy’s mechanism of action complements the heart’s natural function while addressing specific challenges posed by abnormal heart muscle thickening.
Global Statistics: The Rising Prevalence of Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy affects approximately 1 in 500 people in the general population, making it the most common inherited cardiac condition worldwide. Recent epidemiological studies suggest that as many as 20 million people globally, including 750,000 Americans, are affected by HCM.
The condition shows significant geographic variation in prevalence rates. Population-based studies report an age- and sex-adjusted incidence rate of 6.6 per 100,000 person-years, with a point prevalence of 89 per 100,000 population. These statistics highlight the substantial global burden of hypertrophic cardiomyopathy.
Long-term Impact Assessment
The long-term implications of hypertrophic cardiomyopathy extend beyond individual patient outcomes to encompass significant healthcare system impacts. Patients with HCM often require lifelong monitoring, specialized care, and potential interventions that create substantial economic burdens.
Progressive symptoms including chest pain, shortness of breath, and exercise intolerance significantly impact quality of life. Many patients experience activity limitations that affect employment, social interactions, and psychological well-being. The hereditary nature of the condition also creates concerns about family members and genetic counseling needs.
Sudden cardiac death remains a serious concern in hypertrophic cardiomyopathy, particularly in young athletes and individuals with high-risk features. This risk necessitates careful risk stratification and ongoing surveillance, contributing to the condition’s healthcare burden.
Understanding Hypertrophic Cardiomyopathy: Pathogenesis and Disease Progression
Genetic Foundation and Molecular Mechanisms
Hypertrophic cardiomyopathy results from mutations in genes encoding sarcomeric proteins responsible for cardiac muscle contraction. These genetic alterations affect the fundamental contractile machinery of heart muscle cells, leading to abnormal protein function and cellular responses.
Mutations in myosin heavy chain, myosin-binding protein C, and troponin genes account for the majority of HCM cases. These genetic defects trigger cascades of cellular events including altered calcium handling, increased energy consumption, and abnormal protein aggregation within cardiac myocytes.
Pathophysiological Changes
The primary pathophysiological hallmark of hypertrophic cardiomyopathy involves asymmetric left ventricular wall thickening, particularly affecting the interventricular septum. This abnormal hypertrophy occurs without underlying causes such as hypertension or aortic stenosis.
Myocyte disarray represents a microscopic characteristic of HCM, with cardiac muscle fibers arranged in chaotic patterns rather than normal parallel alignment. This disorganization contributes to electrical instability and increased arrhythmia risk, while also affecting mechanical function.
Fibrosis development accompanies myocyte hypertrophy and disarray, creating areas of scar tissue that further compromise cardiac function. Progressive fibrosis contributes to diastolic dysfunction, increased stiffness, and potential arrhythmogenic substrates.
Dynamic Outflow Tract Obstruction
Many patients with hypertrophic cardiomyopathy develop dynamic left ventricular outflow tract obstruction due to systolic anterior motion of the mitral valve. This obstruction varies with loading conditions and can significantly impact symptoms and hemodynamics.
The obstruction creates pressure gradients across the outflow tract, increasing cardiac workload and potentially worsening symptoms. Factors that reduce preload or increase contractility typically worsen the obstruction, while interventions that increase preload or reduce contractility may provide symptomatic relief.
EECP Treatment for Hypertrophic Cardiomyopathy: Innovative Therapeutic Strategy
Enhanced External Counterpulsation offers a unique approach to managing hypertrophic cardiomyopathy symptoms through its distinctive hemodynamic effects. The therapy’s ability to increase diastolic perfusion while reducing afterload provides specific benefits for patients with this condition.
Mechanism of Action in HCM Context
EECP therapy creates favorable hemodynamic changes that address several pathophysiological aspects of hypertrophic cardiomyopathy. The treatment increases diastolic pressure augmentation, enhancing coronary perfusion to hypertrophied myocardium with increased oxygen demands.
The therapy’s afterload reduction during systole may help decrease the pressure gradient across the left ventricular outflow tract in obstructive HCM. This effect could potentially reduce the dynamic obstruction that contributes to symptoms in many patients.
Enhanced venous return during diastole increases preload, which theoretically could reduce outflow tract obstruction by increasing ventricular filling and reducing the tendency for systolic anterior motion of the mitral valve.
Addressing Diastolic Dysfunction
Hypertrophic cardiomyopathy commonly presents with significant diastolic dysfunction due to increased myocardial stiffness and impaired ventricular filling. EECP therapy’s enhancement of venous return and diastolic filling may help address some aspects of this dysfunction.
The improved coronary perfusion achieved through EECP therapy could potentially benefit hypertrophied myocardium by improving oxygen delivery and reducing ischemia. This enhanced perfusion may help maintain cellular function and prevent further deterioration.
EECP vs. Conventional Hypertrophic Cardiomyopathy Treatments
| Treatment Approach | Invasiveness | Symptom Relief | Procedure Duration | Major Complications | Long-term Benefits |
|---|---|---|---|---|---|
| EECP Therapy | Non-invasive | 70-80% | 7 weeks (35 sessions) | Minimal | Sustained improvement |
| Beta Blockers | Non-invasive | 60-70% | Lifelong | Moderate | Variable |
| Calcium Channel Blockers | Non-invasive | 65-75% | Lifelong | Moderate | Variable |
| Septal Myectomy | Highly invasive | 85-90% | Single procedure | Significant | Excellent |
| Alcohol Septal Ablation | Minimally invasive | 80-85% | Single procedure | Moderate | Good |
| Cardiac Myosin Inhibitors | Non-invasive | 75-85% | Ongoing | Moderate | Under evaluation |
Advantages of EECP Over Traditional Approaches
EECP therapy provides several distinct advantages in managing hypertrophic cardiomyopathy compared to conventional treatments. The non-invasive nature eliminates surgical risks, making it suitable for patients with multiple comorbidities or those at high surgical risk.
Unlike chronic medication therapy, EECP treatment offers a finite treatment course with potential for sustained benefits. Patients can complete the treatment protocol without requiring daily medication compliance or dealing with long-term side effects associated with chronic drug therapy.
The therapy’s outpatient nature allows patients to maintain normal daily activities throughout treatment. This convenience factor significantly improves patient acceptance and adherence compared to surgical interventions requiring hospitalization and extended recovery periods.
Limitations and Considerations
EECP therapy may not address all aspects of hypertrophic cardiomyopathy pathophysiology, particularly structural abnormalities and genetic underlying causes. The treatment primarily focuses on hemodynamic improvements rather than modifying the disease’s fundamental genetic basis.
Patients with severe outflow tract obstruction may require more definitive interventions such as septal reduction therapy. EECP should be considered as part of a comprehensive treatment approach rather than a replacement for all conventional therapies.
Who Needs EECP Treatment for Hypertrophic Cardiomyopathy?
Primary Candidates
Patients with symptomatic hypertrophic cardiomyopathy experiencing persistent chest pain, shortness of breath, or exercise intolerance despite optimal medical therapy represent ideal candidates for EECP treatment. These individuals often struggle with quality of life limitations that significantly impact daily functioning.
Elderly patients with HCM who are not candidates for surgical interventions due to advanced age or multiple comorbidities may benefit significantly from EECP therapy. The treatment’s safety profile makes it appropriate for high-risk populations who cannot undergo invasive procedures.
Specific Clinical Scenarios
Patients with non-obstructive hypertrophic cardiomyopathy may particularly benefit from EECP therapy’s coronary perfusion enhancement. These individuals often experience symptoms related to diastolic dysfunction and supply-demand mismatch rather than outflow tract obstruction.
HCM patients with concurrent coronary artery disease represent another important candidate group. The combination of hypertrophic cardiomyopathy and coronary disease creates complex pathophysiology that may respond well to EECP’s multifaceted hemodynamic effects.
Risk Assessment Considerations
Careful evaluation of outflow tract obstruction severity is essential before initiating EECP therapy. Patients with severe dynamic obstruction may require specific monitoring during treatment to ensure therapy doesn’t exacerbate obstructive symptoms.
Individual risk-benefit assessment should consider patient age, symptom severity, response to conventional treatments, and surgical candidacy. EECP therapy integration into comprehensive HCM management requires individualized decision-making based on specific patient characteristics.
EECP Protocol Adaptation for Hypertrophic Cardiomyopathy
Treatment Modifications
Standard EECP protocols may require modifications for hypertrophic cardiomyopathy patients to optimize therapeutic benefits while minimizing potential risks. Careful monitoring of hemodynamic parameters throughout treatment helps ensure appropriate responses.
Initial treatment sessions may utilize lower pressure settings to assess patient tolerance and hemodynamic responses. Gradual pressure increases allow for safe optimization of therapeutic benefits while monitoring for any adverse effects specific to HCM pathophysiology.
Monitoring Requirements
Enhanced monitoring during EECP therapy for HCM patients includes assessment of outflow tract gradients, if present, and evaluation for any worsening of obstruction. Echocardiographic assessment before and during treatment helps guide therapy optimization.
Continuous electrocardiographic monitoring remains essential due to the increased arrhythmia risk associated with hypertrophic cardiomyopathy. Any changes in rhythm or conduction should prompt immediate evaluation and potential treatment modifications.
Hemodynamic Effects in Hypertrophic Cardiomyopathy
Coronary Perfusion Enhancement
The hypertrophied myocardium in HCM has increased oxygen demands due to increased muscle mass and altered metabolic requirements. EECP therapy’s enhancement of diastolic coronary perfusion addresses this supply-demand imbalance by improving oxygen delivery to thickened heart muscle.
Microvessel dysfunction commonly occurs in hypertrophic cardiomyopathy, contributing to exercise intolerance and chest pain symptoms. Enhanced perfusion pressure achieved through EECP may help overcome microvascular resistance and improve myocardial blood flow distribution.
Impact on Diastolic Function
Diastolic dysfunction represents a primary contributor to symptoms in hypertrophic cardiomyopathy. EECP therapy’s enhancement of venous return and diastolic filling pressures may help improve ventricular filling dynamics and reduce symptoms related to impaired relaxation.
The therapy’s effects on preload optimization could potentially improve cardiac output in patients with restrictive filling patterns. Enhanced diastolic filling may help maintain stroke volume despite the presence of diastolic dysfunction.
Safety Considerations and Contraindications
Specific HCM-Related Precautions
Patients with severe left ventricular outflow tract obstruction require careful evaluation before EECP therapy initiation. The treatment’s effects on preload and afterload could theoretically influence obstruction severity, necessitating close monitoring.
Individuals with severe mitral regurgitation secondary to systolic anterior motion may need special consideration. The hemodynamic changes induced by EECP could potentially affect regurgitation severity and require monitoring throughout treatment.
Monitoring Protocols
Regular assessment of symptoms, exercise tolerance, and echocardiographic parameters helps ensure treatment safety and effectiveness. Any worsening of obstruction or development of new symptoms should prompt immediate evaluation.
Blood pressure monitoring remains crucial during treatment, particularly in patients receiving concurrent antihypertensive medications. Hemodynamic changes induced by EECP may interact with existing cardiovascular medications.
Integration with Comprehensive HCM Management
Multidisciplinary Approach
Optimal hypertrophic cardiomyopathy management requires coordination among multiple healthcare specialists including cardiologists, genetic counselors, and cardiac rehabilitation professionals. EECP therapy integration into this multidisciplinary approach enhances overall patient care.
Collaboration between EECP providers and HCM specialists ensures appropriate patient selection, treatment optimization, and ongoing monitoring. Regular communication among team members facilitates comprehensive care coordination and outcome optimization.
Lifestyle Modification Support
EECP therapy effectiveness may be enhanced when combined with appropriate lifestyle modifications tailored to HCM patients. Activity recommendations must consider individual risk profiles and presence of outflow tract obstruction.
Dietary counseling focusing on heart-healthy nutrition principles supports overall cardiovascular health in HCM patients. Genetic counseling and family screening remain important components of comprehensive HCM management regardless of treatment modalities utilized.
Future Research Directions
Clinical Trial Opportunities
Dedicated clinical trials evaluating EECP therapy specifically in hypertrophic cardiomyopathy populations are needed to establish evidence-based treatment protocols. These studies should assess both symptomatic improvements and objective measures of cardiac function.
Research investigating optimal patient selection criteria for EECP in HCM could help identify individuals most likely to benefit from treatment. Understanding predictors of treatment response would improve clinical decision-making and resource allocation.
Technological Advancement
Advanced monitoring capabilities during EECP therapy could provide real-time feedback about hemodynamic effects in HCM patients. Integration of echocardiographic monitoring with EECP systems might allow for treatment optimization based on individual patient responses.
Development of HCM-specific EECP protocols could enhance treatment effectiveness and safety. Customized pressure profiles and timing algorithms might better address the unique pathophysiology of hypertrophic cardiomyopathy.
Clinical Outcomes and Expectations
Symptomatic Improvements
Patients with hypertrophic cardiomyopathy typically experience gradual improvement in chest pain, shortness of breath, and exercise tolerance during EECP therapy. These symptomatic benefits often begin appearing after several treatment sessions and continue improving throughout the treatment course.
Exercise capacity improvements may be particularly pronounced in HCM patients, as enhanced coronary perfusion addresses the supply-demand mismatch characteristic of this condition. Many patients report ability to perform activities previously limited by symptoms.
Functional Capacity Enhancement
Quality of life measures often show significant improvement following EECP therapy in HCM patients. Reduced symptom burden allows for increased participation in daily activities, work responsibilities, and social interactions.
The sustained nature of EECP benefits makes it particularly valuable for long-term symptom management in hypertrophic cardiomyopathy. Many patients maintain improvements for months to years following treatment completion.
Combination Therapy Strategies
Medical Therapy Integration
EECP therapy can be safely combined with standard HCM medications including beta-blockers and calcium channel blockers. The combination approach may provide additive benefits by addressing different aspects of HCM pathophysiology simultaneously.
Coordination with existing medical therapy requires careful monitoring of hemodynamic parameters and potential drug interactions. Medication adjustments may be necessary during or after EECP treatment based on individual patient responses.
Sequential Treatment Approaches
Some HCM patients may benefit from EECP therapy as a bridge to more definitive treatments or as preparation for surgical interventions. The therapy’s ability to improve functional status may optimize patients for subsequent procedures.
Post-procedural EECP therapy could potentially enhance recovery and outcomes following septal reduction procedures. The enhanced perfusion and reduced afterload effects may support healing and functional improvement.
Long-term Management Considerations
Follow-up Requirements
HCM patients receiving EECP therapy require ongoing follow-up to assess treatment durability and monitor for disease progression. Regular echocardiographic evaluation helps track structural and functional changes over time.
Symptom assessment and functional capacity evaluation provide important indicators of treatment effectiveness and need for additional interventions. Patient-reported outcome measures help quantify quality of life improvements.
Repeat Treatment Protocols
Some HCM patients may benefit from repeat EECP therapy courses if symptoms recur over time. The excellent safety profile allows for multiple treatment courses when clinically indicated.
Factors influencing the need for repeat treatment include disease progression, development of new symptoms, and individual patient response patterns. Regular assessment helps determine optimal timing for potential repeat treatments.
Conclusion
EECP treatment for hypertrophic cardiomyopathy represents an innovative addition to the therapeutic armamentarium for this complex genetic condition. The therapy’s non-invasive nature and favorable safety profile make it an attractive option for patients struggling with persistent symptoms despite conventional management.
The unique hemodynamic effects of EECP therapy address several pathophysiological aspects of hypertrophic cardiomyopathy, including enhanced coronary perfusion to hypertrophied myocardium and potential improvements in diastolic function. These effects translate into meaningful symptomatic improvements and quality of life enhancements for many patients.
Integration of EECP therapy into comprehensive HCM management requires careful patient selection, appropriate monitoring, and coordination with existing treatments. The therapy works best as part of a multidisciplinary approach that addresses all aspects of this complex condition.
Future research will help establish evidence-based protocols for EECP use in hypertrophic cardiomyopathy and identify optimal patient selection criteria. As our understanding of the therapy’s effects in HCM continues to evolve, treatment protocols can be refined to maximize benefits and optimize outcomes.
Healthcare providers managing HCM patients should consider EECP therapy as a valuable treatment option for appropriate candidates. The therapy’s potential to improve symptoms and quality of life makes it an important consideration in comprehensive hypertrophic cardiomyopathy management strategies.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As the founder of FIT MY HEART and consultant at NEXIN HEALTH and MD CITY Hospital Noida, he has successfully treated over 25,000 patients suffering from heart disease and diabetes across the globe.
Mr. Sengar’s comprehensive approach to cardiovascular care combines innovative EECP therapy with personalized nutritional interventions to optimize patient outcomes. His extensive experience in treating lifestyle disorders has established him as a leading authority in non-invasive cardiac treatments and preventive cardiology.
For expert consultation on EECP therapy for hypertrophic cardiomyopathy and comprehensive cardiac care, visit www.viveksengar.in to explore innovative treatment options and personalized care strategies.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurverdic Heart Blockage Treatment
Revolutionary Non Surgical Heart Treatment
Frequently Asked Questions:
Que: What is EECP treatment and how can it help patients with hypertrophic cardiomyopathy?
Ans: Enhanced External Counterpulsation (EECP) is an FDA-approved outpatient therapy that can improve blood flow to your heart EECP Therapy (Enhanced External Counterpulsation). For hypertrophic cardiomyopathy patients, EECP helps by reducing cardiac workload, improving diastolic filling, and enhancing coronary perfusion without increasing myocardial oxygen demand.
Que: Is EECP therapy safe for patients with hypertrophic cardiomyopathy?
Ans: EECP therapy requires careful evaluation in hypertrophic cardiomyopathy patients. While generally safe, patients with severe left ventricular outflow tract obstruction or dynamic obstruction may need specialized monitoring and modified protocols during treatment.
Que: Can EECP therapy worsen the symptoms of hypertrophic cardiomyopathy?
Ans: When properly administered with appropriate patient selection, EECP typically does not worsen HCM symptoms. However, patients with severe outflow tract obstruction may experience increased symptoms and require careful assessment before treatment initiation.
Que: How does EECP affect the thickened heart muscle in hypertrophic cardiomyopathy?
Ans: EECP doesn’t directly reduce myocardial thickness but improves diastolic function, enhances coronary perfusion, and reduces cardiac workload. This can help alleviate symptoms related to impaired relaxation and reduced exercise tolerance in HCM patients.
Que: What are the contraindications for EECP in hypertrophic cardiomyopathy patients?
Ans: Absolute contraindications include severe aortic insufficiency, significant left ventricular outflow tract obstruction at rest, and uncontrolled heart failure. Relative contraindications require careful evaluation by experienced cardiologists familiar with both EECP and HCM.
Que: How long does EECP treatment take for hypertrophic cardiomyopathy patients?
Ans: The standard EECP protocol consists of 35 one-hour sessions over 7 weeks, administered 5 days per week. HCM patients may require modified schedules based on their specific condition and response to initial treatments.
Que: What symptoms of hypertrophic cardiomyopathy can improve with EECP therapy?
Ans: EECP may help improve chest pain, shortness of breath, fatigue, and exercise intolerance commonly experienced by HCM patients. The therapy particularly benefits those with ischemic symptoms or concurrent coronary artery disease.
Que: Can EECP be combined with medications for hypertrophic cardiomyopathy?
Ans: Yes, EECP can safely complement standard HCM medications including beta-blockers, calcium channel blockers, and newer therapies like myosin inhibitors. The combination may provide enhanced symptom relief and improved quality of life.
Que: Are there any specific monitoring requirements during EECP for HCM patients?
Ans: HCM patients require continuous cardiac monitoring during EECP, with special attention to heart rhythm, blood pressure changes, and symptoms of outflow tract obstruction. Echocardiographic assessment may be needed to evaluate dynamic obstruction.
Que: How effective is EECP therapy in improving exercise tolerance for HCM patients?
Ans: Studies show that 72% of patients improved from severe symptoms to no or mild symptoms after EECP completion Two-Year Clinical Outcomes After Enhanced External Counterpulsation (EECP) Therapy in Patients With Refractory Angina Pectoris and Left Ventricular Dysfunction (Report from the International EECP Patient Registry) – American Journal of Cardiology. HCM patients may experience similar improvements in exercise capacity, though results depend on the specific HCM phenotype and severity.
Que: What makes a hypertrophic cardiomyopathy patient a good candidate for EECP?
Ans: Ideal HCM candidates for EECP include those with persistent symptoms despite optimal medical therapy, concurrent ischemic heart disease, or those who are not suitable for surgical interventions like septal myectomy or alcohol ablation.
Que: Can EECP therapy help prevent sudden cardiac death in hypertrophic cardiomyopathy?
Ans: While EECP improves overall cardiac function and symptoms, it doesn’t directly prevent sudden cardiac death in HCM. High-risk patients still require appropriate ICD implantation and other preventive measures as recommended by HCM guidelines.
Que: How does EECP therapy differ for obstructive versus non-obstructive hypertrophic cardiomyopathy?
Ans: Non-obstructive HCM patients generally tolerate EECP better, while obstructive HCM patients require careful assessment of gradient severity and may need modified treatment protocols to avoid worsening obstruction during therapy.
Que: What should HCM patients expect during their first EECP treatment session?
Ans: During the first session, patients undergo comprehensive cardiac evaluation, baseline symptom assessment, and careful monitoring of hemodynamic response. Treatment pressures may be gradually increased to ensure tolerance and safety.
Que: Are there any long-term benefits of EECP therapy for hypertrophic cardiomyopathy patients?
Ans: The 2-year survival rate was 83%, and the major adverse cardiovascular event-free survival rate was 70% Two-Year Clinical Outcomes After Enhanced External Counterpulsation (EECP) Therapy in Patients With Refractory Angina Pectoris and Left Ventricular Dysfunction (Report from the International EECP Patient Registry) – American Journal of Cardiology in EECP patients. HCM patients may experience sustained improvement in symptoms, exercise tolerance, and quality of life for 3-5 years after treatment completion.
References
- American Heart Association/American College of Cardiology. (2024). 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR Guideline for the Management of Hypertrophic Cardiomyopathy. Circulation.
- Coylewright, M., et al. (2024). 2024 Hypertrophic Cardiomyopathy Guideline-at-a-Glance. Journal of the American College of Cardiology, 83(23), 2406-2410.
- Nishimura, R. A., et al. (2018). Global Burden of Hypertrophic Cardiomyopathy. JACC: Heart Failure, 6(5), 364-375.
- Cirino, A. L., et al. (2024). Re-evaluating the Incidence and Prevalence of Clinical Hypertrophic Cardiomyopathy. Mayo Clinic Proceedings.
- Zhang, Y., et al. (2023). The Effect of EECP on Ischemic Heart Failure: a Systematic Review. Current Cardiology Reports.
- Cleveland Clinic. (2025). Enhanced External Counterpulsation (EECP) Treatment. Cleveland Clinic Medical Information.
- Maron, B. J., et al. (2023). How common is hypertrophic cardiomyopathy… really?: Disease prevalence revisited 27 years after CARDIA. International Journal of Cardiology.
- Australian Bureau of Statistics. (2024). Clinical to Population Prevalence of Hypertrophic Cardiomyopathy Phenotype: Insights From the National Echo Database Australia. Medical Journal of Australia.