EECP Treatment for Heart Failure: Heart failure continues to challenge millions worldwide, but innovative treatments like Enhanced External Counterpulsation (EECP) are transforming how we approach this complex condition. This breakthrough therapy offers hope for patients seeking alternatives to traditional invasive procedures.
Heart failure affects your body’s ability to pump blood effectively, leading to symptoms that can dramatically impact your quality of life. Traditional treatment methods often involve medications, lifestyle changes, and sometimes surgical interventions. However, EECP therapy presents a unique, non-invasive solution that works by improving blood circulation throughout your cardiovascular system.
Recent clinical studies demonstrate that EECP treatment significantly enhances cardiac function while reducing symptoms in heart failure patients. This therapeutic approach utilizes external pressure to optimize blood flow, creating natural bypasses around blocked arteries. The therapy’s effectiveness lies in its ability to stimulate your body’s own healing mechanisms without requiring surgical intervention.
Global Heart Failure Statistics: Understanding the Magnitude
Approximately 6.7 million Americans over the age of 20 currently live with heart failure, a figure projected to rise to 8.7 million by 2030, 10.3 million by 2040, and a staggering 11.4 million by 2050. These statistics highlight the urgent need for effective treatment options like EECP therapy.
The current worldwide prevalence of HF is estimated at 64.34 million cases (8.52 per 1,000 inhabitants, 29% of which mild, 19% moderate and 51% severe HF). This global burden demonstrates why innovative treatments such as enhanced external counterpulsation are becoming increasingly important in modern cardiology.
The economic impact of heart failure extends beyond individual suffering. Healthcare systems worldwide spend billions annually on heart failure management, making cost-effective treatments like EECP therapy essential for sustainable cardiac care. Countries with aging populations face particularly challenging increases in heart failure prevalence.
Long-term Impact of Rising Heart Failure Rates:
Heart failure mortality rates continue climbing globally. In 2002, the HF mortality was 3.0 per 100,000 persons, which rose to 15.6 per 100,000 persons in 2020. This upward trend emphasizes the critical importance of accessible treatments like EECP for heart failure patients.
The societal burden includes reduced productivity, increased disability claims, and strain on caregiving resources. Families often struggle with the emotional and financial challenges of supporting loved ones with heart failure. EECP treatment offers hope by potentially reducing hospitalizations and improving functional capacity.
Young adults between ages 15-44 show increasing heart failure rates, challenging traditional assumptions about this condition affecting only older populations. This demographic shift requires innovative treatment approaches that can accommodate younger patients’ lifestyle needs while providing effective cardiac support.
Understanding Heart Failure: Clinical Pathways and Disease Progression
Heart failure represents a complex syndrome where your heart cannot pump blood efficiently to meet your body’s demands. The pathogenesis involves multiple interconnected mechanisms that progressively compromise cardiac function over time.
Initial Cardiac Injury Phase:
The disease typically begins with an initial insult to your heart muscle. Common triggers include myocardial infarction, hypertension, viral infections, or genetic predispositions. During this phase, your heart attempts to compensate through various mechanisms including increased heart rate and enlarged chamber size.
Neurohormonal activation occurs early in the disease process. Your body releases hormones like adrenaline and angiotensin II to maintain blood pressure and cardiac output. Initially helpful, these compensatory mechanisms eventually become detrimental, leading to further cardiac damage and symptom progression.
Ventricular Remodeling Stage:
As heart failure progresses, structural changes occur in your heart chambers. The left ventricle often enlarges and changes shape, becoming less efficient at pumping blood. This remodeling process involves changes at the cellular level, including myocyte death and replacement with scar tissue.
Vascular changes accompany cardiac remodeling. Your blood vessels become less responsive to normal regulatory signals, contributing to increased afterload and reduced exercise capacity. These changes explain why treatments like EECP therapy, which improve vascular function, can be particularly beneficial.
Advanced Heart Failure Complications:
In advanced stages, multiple organ systems become affected. Your kidneys may develop dysfunction due to reduced blood flow, leading to fluid retention and worsening symptoms. The liver can become congested, affecting its ability to process medications and maintain protein synthesis.
Pulmonary complications develop as pressure backs up into your lungs, causing shortness of breath and reduced exercise tolerance. This complex interplay of organ dysfunction explains why comprehensive treatments addressing multiple pathways, such as EECP therapy, often prove more effective than single-target approaches.
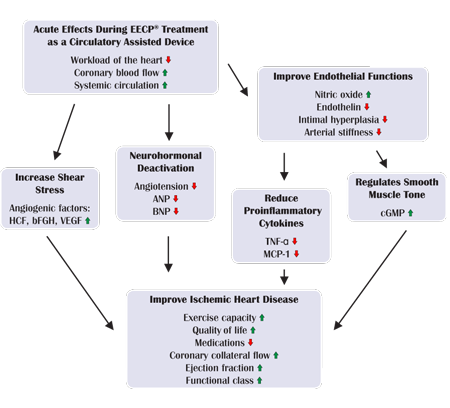
How EECP Treatment Works: Mechanisms of Action
Enhanced external counterpulsation operates on sophisticated physiological principles that harness your body’s natural circulatory mechanisms. Understanding these mechanisms helps explain why EECP therapy proves effective for heart failure patients.
Counterpulsation Principle:
EECP therapy synchronizes with your cardiac cycle using electrocardiogram monitoring. During diastole (when your heart relaxes), pneumatic cuffs inflate sequentially from your legs upward, pushing blood toward your heart and vital organs. This external assistance effectively increases diastolic pressure and coronary perfusion.
During systole (when your heart contracts), the cuffs rapidly deflate, reducing afterload and making it easier for your heart to pump blood. This synchronized assistance reduces cardiac workload while improving overall circulation, particularly beneficial for heart failure patients with compromised pumping function.

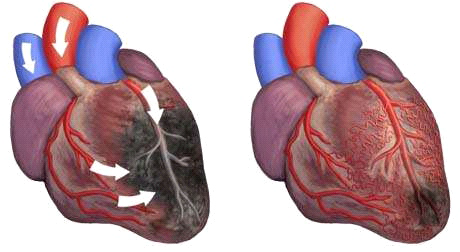
Principal of EECP
Vascular Adaptations:
Regular EECP sessions stimulate the development of collateral circulation. Your body responds to the improved blood flow by growing new blood vessels and enhancing existing ones. This process, called angiogenesis, creates natural bypasses around blocked or narrowed arteries.
Endothelial function improves with EECP treatment. The cells lining your blood vessels become more responsive to vasodilating signals, improving your overall vascular health. Enhanced endothelial function contributes to better blood pressure control and reduced cardiovascular risk.
Neurohormonal Benefits:
EECP therapy influences your body’s neurohormonal balance in ways that benefit heart failure patients. The treatment can reduce sympathetic nervous system activity, leading to lower heart rates and blood pressure. This neurohormonal rebalancing helps break the cycle of progressive heart failure deterioration.
Inflammatory markers often decrease with EECP treatment. Chronic inflammation contributes to heart failure progression, so reducing inflammatory activity through EECP therapy may help slow disease advancement while improving symptoms and quality of life.
EECP vs. Traditional Heart Failure Treatments: Comprehensive Comparison
| Treatment Aspect | EECP Therapy | Medication Management | Surgical Interventions |
|---|---|---|---|
| Invasiveness | Non-invasive, outpatient | Non-invasive, daily medications | Invasive, requires hospitalization |
| Treatment Duration | 35 – 40 sessions over 7 weeks | Lifelong adherence required | Single procedure with recovery time |
| Side Effects | Minimal, temporary skin irritation | Multiple drug interactions, organ toxicity | Surgical risks, infection, bleeding |
| Effectiveness Rate | 69% of patients improved by at least 1 Canadian Cardiovascular Society (CCS) angina class | Variable, depends on medication tolerance | High success rates but limited candidates |
| Long-term Benefits | Over 92% had sustained improvement at 1-year follow-up | Requires continuous medication adjustment | Durable results for suitable candidates |
| Patient Comfort | Comfortable, no anesthesia needed | Daily pill burden, potential side effects | Post-operative pain and recovery period |
| Contraindications | Few absolute contraindications | Multiple drug allergies and interactions | Extensive medical clearance required |
| Monitoring Requirements | Basic vital signs during treatment | Regular blood tests, organ function monitoring | Intensive post-operative monitoring |
Combination Therapy Advantages:
EECP treatment works synergistically with conventional heart failure medications. Patients often experience enhanced benefits when combining EECP with optimized medical therapy. This integrated approach addresses multiple pathways contributing to heart failure progression.
The non-competitive nature of EECP allows it to complement other treatments without interfering with their mechanisms. Unlike some therapies that may contraindicate others, EECP enhances overall treatment effectiveness while maintaining safety profiles.
Quality of Life Improvements:
The standard course of EECP is safe in patients with IHF and can significantly improve the quality of life of these patients. This improvement often exceeds what patients experience with medications alone, particularly regarding exercise tolerance and daily activity levels.
Psychological benefits accompany physical improvements with EECP therapy. Patients often report reduced anxiety about their condition and increased confidence in their ability to manage daily activities. These psychological improvements contribute significantly to overall treatment success.
Who Needs EECP Treatment for Heart Failure?
EECP therapy benefits a diverse range of heart failure patients, though specific criteria help identify optimal candidates. Understanding these criteria ensures patients receive appropriate evaluation for this innovative treatment option.
Primary Candidates:
Patients with ischemic heart failure represent the largest group benefiting from EECP treatment. These individuals typically have underlying coronary artery disease contributing to their heart failure symptoms. EECP’s ability to improve coronary circulation makes it particularly effective for this population.
Individuals experiencing persistent symptoms despite optimal medical therapy often find significant relief with EECP. When conventional treatments reach their limits, EECP provides an additional therapeutic option that can meaningfully improve quality of life and functional capacity.
Specific Clinical Scenarios:
Patients who are not candidates for surgical revascularization due to high operative risk or unsuitable anatomy benefit greatly from EECP therapy. This non-invasive alternative provides circulatory benefits without surgical risks, making it ideal for high-risk populations.
Heart failure patients with preserved ejection fraction often respond well to EECP treatment. While their heart’s pumping function may appear normal, these patients experience symptoms related to impaired relaxation and filling, which EECP can help address through improved circulation.
Age and Functional Considerations:
Elderly patients with multiple comorbidities frequently prove excellent EECP candidates. The treatment’s non-invasive nature makes it suitable for frail individuals who cannot tolerate more aggressive interventions. Age alone does not contraindicate EECP therapy.
Younger patients seeking to maintain active lifestyles while managing heart failure find EECP particularly appealing. The treatment schedule allows continued work and family responsibilities while providing significant symptom improvement and enhanced exercise capacity.
Contraindications to Consider:
Certain conditions preclude EECP treatment. Active infections, severe peripheral vascular disease, and certain arrhythmias may contraindicate therapy. Pregnancy represents an absolute contraindication due to unknown effects on fetal development.
Severe hypertension requires control before initiating EECP treatment. Patients with blood pressure above 180/110 mmHg need optimization of antihypertensive therapy before beginning EECP sessions to ensure safety and effectiveness.
Clinical Benefits of EECP in Heart Failure Management
EECP therapy provides multiple clinical benefits that extend beyond simple symptom relief. These advantages make it an valuable component of comprehensive heart failure management strategies.
Hemodynamic Improvements:
EECP treatment enhances cardiac output through improved diastolic filling and reduced afterload. Patients often experience measurable improvements in exercise capacity and reduced fatigue during daily activities. These hemodynamic benefits translate into meaningful functional improvements.
Blood pressure optimization occurs with regular EECP sessions. The treatment helps stabilize both systolic and diastolic pressures, potentially reducing medication requirements in some patients. This blood pressure improvement contributes to overall cardiovascular risk reduction.
Symptom Relief Patterns:
Shortness of breath, one of the most distressing heart failure symptoms, often improves significantly with EECP therapy. Patients report being able to climb stairs, walk longer distances, and perform daily activities with less respiratory distress.
Fatigue reduction represents another major benefit of EECP treatment. The improved circulation helps deliver oxygen and nutrients more efficiently throughout the body, resulting in increased energy levels and enhanced quality of life for heart failure patients.
Functional Capacity Enhancement:
Exercise tolerance typically improves markedly with EECP therapy. Patients often progress from severely limited activity to being able to perform moderate exercise. This improvement in functional capacity has profound implications for independence and quality of life.
Sleep quality frequently improves following EECP treatment. Better circulation and reduced fluid retention often lead to decreased nocturnal symptoms, allowing for more restful sleep patterns that further enhance overall well-being.
EECP Treatment Protocol and Procedure Details
Understanding the EECP treatment process helps patients prepare for therapy and know what to expect during their treatment course. The standardized protocol ensures consistent delivery of therapeutic benefits.
Treatment Schedule:
Standard EECP therapy consists of 35 – 40 one-hour sessions administered over seven weeks. Sessions typically occur five days per week, allowing weekends for rest and recovery. This schedule provides optimal therapeutic benefit while accommodating most patients’ lifestyle needs.
Each session involves lying comfortably on a treatment bed while pneumatic cuffs are applied to your legs and lower torso. The treatment is pain-free and many patients find it relaxing, often using the time to read, listen to music, or rest.
Session Procedures:
Before each session, medical staff monitors your vital signs and reviews any changes in your condition. Electrocardiogram electrodes are placed to synchronize the EECP device with your heartbeat, ensuring optimal timing of the counterpulsation cycles.
During treatment, the device inflates cuffs sequentially from your calves to your thighs and buttocks during diastole, then rapidly deflates during systole. Pressure settings are adjusted based on your tolerance and clinical response to optimize therapeutic benefit.
Monitoring and Safety:
Continuous monitoring during EECP sessions ensures patient safety and treatment effectiveness. Medical staff observe vital signs, patient comfort, and treatment parameters throughout each session, making adjustments as needed to maintain optimal therapy delivery.
Progressive assessment occurs weekly to evaluate treatment response and make any necessary protocol modifications. This ongoing evaluation ensures patients receive maximum benefit from their EECP therapy course while maintaining safety standards.
Scientific Evidence Supporting EECP for Heart Failure
Robust clinical research supports EECP therapy’s effectiveness in heart failure management. Multiple studies demonstrate significant improvements in patient outcomes and quality of life measures.
Registry Data Analysis:
Data from the International EECP Patient Registry indicate that 69% of patients improved by at least 1 Canadian Cardiovascular Society (CCS) angina class immediately after EECP. This improvement rate demonstrates EECP’s consistent effectiveness across diverse patient populations.
Long-term follow-up data strengthens the evidence for EECP’s durability. Of these patients, 72% had sustained improvement at 1-year follow-up. This sustained benefit suggests that EECP provides lasting therapeutic value rather than temporary symptom relief.
Systematic Review Findings:
According to the existing evidence, the standard course of EECP is safe in patients with IHF and can significantly improve the quality of life of these patients. This systematic review conclusion provides high-level evidence supporting EECP’s role in heart failure management.
Safety profiles consistently demonstrate EECP’s excellent tolerability across multiple studies. Serious adverse events remain rare, making EECP an attractive option for patients who may not tolerate more aggressive interventions.
Hospitalization Reduction:
Studies examining healthcare utilization show promising trends toward reduced hospitalizations following EECP therapy. 9% of patients underwent EECP and 13.6% of controls were readmitted within 180 days. This reduction in readmission rates suggests EECP may help stabilize patients and reduce healthcare costs.
Emergency department visits often decrease following successful EECP treatment courses. Patients report feeling more confident managing their symptoms and experience fewer acute exacerbations requiring urgent medical attention.
Integration with Comprehensive Heart Failure Care
EECP therapy works best when integrated into comprehensive heart failure management programs. This coordinated approach addresses multiple aspects of the condition while optimizing overall patient outcomes.
Multidisciplinary Team Approach:
Successful EECP integration requires coordination between cardiologists, EECP specialists, nurses, and rehabilitation professionals. Each team member contributes unique expertise to ensure patients receive comprehensive care throughout their treatment journey.
Patient education remains crucial for successful EECP integration. Understanding how EECP complements other treatments helps patients maintain adherence to all aspects of their care plan while maximizing therapeutic benefits.
Lifestyle Modification Support:
EECP therapy often enhances patients’ ability to participate in cardiac rehabilitation and exercise programs. Improved exercise tolerance following EECP treatment creates opportunities for further cardiovascular conditioning and lifestyle improvements.
Nutritional counseling becomes more effective when combined with EECP therapy. Patients often find they have increased energy to prepare healthy meals and maintain better dietary habits as their symptoms improve with treatment.
Medication Optimization:
EECP therapy may allow for optimization of heart failure medications. Some patients experience improved tolerance of evidence-based therapies following EECP treatment, potentially enhancing overall medical management effectiveness.
Regular monitoring during EECP treatment provides opportunities to assess medication effectiveness and make necessary adjustments. This ongoing evaluation ensures patients receive optimal medical therapy alongside their EECP treatment course.
Future Directions in EECP Research
Ongoing research continues to expand our understanding of EECP therapy’s potential applications and mechanisms. These investigations may lead to enhanced treatment protocols and broader therapeutic applications.
Emerging Applications:
Research into EECP’s effects on different types of heart failure continues evolving. Studies examining heart failure with preserved ejection fraction show promising preliminary results, potentially expanding EECP’s therapeutic applications.
Combination therapies incorporating EECP with newer heart failure treatments represent an active area of investigation. These studies may identify synergistic effects that enhance overall treatment effectiveness.
Mechanism Studies:
Advanced imaging techniques are providing new insights into EECP’s cardiovascular effects. Studies using cardiac MRI and other sophisticated technologies help clarify how EECP improves cardiac function and symptom relief.
Biomarker research examines how EECP therapy affects inflammatory markers, neurohormonal activation, and other cardiac biomarkers. These studies may help identify patients most likely to benefit from EECP treatment.
Technology Advances:
Device improvements continue enhancing EECP delivery and patient comfort. New cuff designs and pressure control systems may improve treatment effectiveness while reducing any minor discomfort associated with therapy.
Remote monitoring capabilities are being investigated to enhance patient safety and treatment optimization. These technological advances may allow for more personalized EECP protocols based on individual patient responses.
Patient Selection and Evaluation Process
Proper patient selection ensures optimal EECP outcomes while maintaining safety standards. Comprehensive evaluation helps identify patients most likely to benefit from this innovative therapy.
Initial Assessment:
Thorough cardiovascular evaluation precedes EECP therapy initiation. This assessment includes detailed history, physical examination, electrocardiogram, and echocardiogram to characterize heart failure severity and identify any contraindications.
Exercise testing when appropriate helps establish baseline functional capacity and provides objective measures for monitoring treatment response. These baseline measurements prove valuable for documenting EECP therapy’s effectiveness.
Risk Stratification:
Patient risk assessment considers both cardiac and non-cardiac factors that might influence EECP therapy success. High-risk patients may require additional monitoring or modified treatment protocols to ensure safety.
Comorbidity evaluation examines conditions that might affect EECP tolerance or effectiveness. Certain conditions may require optimization before initiating EECP therapy to maximize treatment benefits.
Treatment Planning:
Individualized treatment plans consider patient-specific factors including symptom severity, functional limitations, and treatment goals. This personalized approach helps ensure EECP therapy addresses each patient’s unique needs and circumstances.
Patient education and expectation setting form crucial components of treatment planning. Understanding EECP therapy’s realistic benefits and timeline helps patients maintain appropriate expectations and treatment adherence.
Conclusion: EECP’s Role in Modern Heart Failure Care
EECP treatment for heart failure represents a significant advancement in non-invasive cardiac therapy. The evidence consistently demonstrates meaningful improvements in symptoms, quality of life, and functional capacity for appropriately selected patients.
The therapy’s excellent safety profile makes it suitable for many patients who cannot tolerate more aggressive interventions. Combined with its effectiveness and non-invasive nature, EECP provides valuable therapeutic option for comprehensive heart failure management.
As heart failure prevalence continues rising globally, treatments like EECP become increasingly important for managing this complex condition. The therapy’s ability to complement existing treatments while providing unique benefits positions it as a valuable component of modern cardiovascular care.
Future research will likely expand EECP applications and enhance treatment protocols. This ongoing development ensures that EECP therapy will continue evolving to meet the growing needs of heart failure patients worldwide.
About the Author
Mr. Vivek Singh Sengar is a distinguished clinical nutritionist and researcher with specialized expertise in EECP therapy and clinical nutrition. As an expert in treating patients with lifestyle disorders, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar serves as the Founder of FIT MY HEART and works as a Consultant at NEXIN HEALTH and MD CITY Hospital Noida. His extensive experience in cardiovascular care and innovative non-surgical treatment approaches makes him a leading authority in integrated EECP therapy applications combined with holistic healing methods.
His practice focuses on providing comprehensive alternatives to traditional cardiac interventions, helping patients achieve optimal cardiovascular health through evidence-based non-surgical treatments combined with lifestyle optimization and natural healing approaches.
For more information about integrated non-surgical cardiac treatments and comprehensive cardiovascular health services, visit www.viveksengar.in.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Ayurvedic Heart Blockage Treatment
Revolutionary Non-Surgical Heart Treatment
EECP Treatment for Heart Failure: A Revolutionary Non-Invasive Approach to Cardiac Recovery
Frequently Asked Questions:
Que: What is EECP treatment in the context of heart failure?
Ans: EECP (Enhanced External Counter Pulsation) is a non-invasive therapy that helps improve blood flow to the heart, enhancing cardiac function in heart failure patients.
Que: How does EECP help in heart failure recovery?
Ans: EECP increases oxygen-rich blood flow to the heart, reduces cardiac workload, and supports the development of collateral arteries for better heart function.
Que: Is EECP suitable for all heart failure patients?
Ans: EECP is ideal for stable heart failure patients, especially those with low ejection fraction and persistent symptoms despite medication.
Que: Can EECP improve low ejection fraction in heart failure patients?
Ans: Yes, EECP has shown significant improvement in LVEF (Left Ventricular Ejection Fraction) in many heart failure cases.
Que: How many EECP sessions are needed for visible improvement?
Ans: Typically, 35–40 sessions over 6–7 weeks are recommended for best results in heart failure patients.
Que: Is EECP a cure for heart failure?
Ans: No, EECP is not a cure but a powerful supportive therapy that helps manage and reverse symptoms when combined with lifestyle and medication.
Que: Does EECP reduce the need for surgery or transplant?
Ans: In many cases, EECP reduces the need for bypass surgery or heart transplant by improving cardiac performance non-invasively.
Que: Are there any risks or side effects with EECP in heart failure?
Ans: EECP is generally safe. Minor side effects like leg soreness or mild bruising can occur but are temporary.
Que: How soon can heart failure patients feel relief after EECP?
Ans: Some patients experience relief from breathlessness and fatigue within 2–3 weeks, with maximum benefits after completing the therapy cycle.
Que: Can EECP be used alongside other heart failure treatments?
Ans: Yes, EECP complements medications, dietary changes, and other therapies in a comprehensive heart failure recovery plan.
Que: Is EECP treatment painful?
Ans: No, EECP is painless. Patients lie comfortably while leg cuffs inflate rhythmically to assist blood flow.
Que: Who should avoid EECP treatment in heart failure?
Ans: Patients with uncontrolled high blood pressure, bleeding disorders, or severe aortic valve disease may not be suitable candidates.
Que: Is EECP FDA-approved for heart failure treatment?
Ans: Yes, EECP is FDA-approved for angina and heart failure with proper indications and guidelines.
Que: Where is EECP therapy available in India?
Ans: EECP therapy is available at non-invasive cardiology centers, advanced rehab clinics, and heart hospitals across major Indian cities.
Que: Can EECP be repeated if heart failure symptoms return?
Ans: Yes, EECP is safe to repeat and is often used periodically for long-term heart failure management.