Vitamin B12 Deficiency is a silent health crisis that affects millions of people worldwide, especially those managing chronic conditions like heart disease and diabetes. Vitamin B12, also known as cobalamin, is a vital nutrient that your body cannot produce on its own. It acts as a spark plug for your metabolism, helping your body create DNA and maintain the protective coating around your nerves. When your levels drop, it can lead to Vitamin B12 Deficiency, causing a breakdown in how your heart, brain, and blood function. For patients with metabolic disorders, maintaining the right balance of this vitamin is not just about nutrition; it is about preventing serious long-term complications.
Fact Sheet: Surprising Truths About Vitamin B12
-
The 5-Year Storage: Unlike most water-soluble vitamins that leave your body daily, your liver can store enough B12 to last 3 to 5 years. This means Vitamin B12 Deficiency symptoms often take years to show up.
-
The “Brain Shrinkage” Link: Recent clinical trials suggest that chronic Vitamin B12 Deficiency can actually lead to brain volume loss, mimicking the signs of early dementia.
-
Heart Connection: Low B12 levels cause a rise in Homocysteine, an amino acid that damages the lining of your arteries, significantly increasing the risk of heart attacks and strokes.
-
Metformin Interaction: According to a Harvard study, nearly 30% of diabetes patients taking Metformin long-term develop a mild Vitamin B12 Deficiency because the medicine blocks absorption.
-
The “Big Cell” Anemia: In Vitamin B12 Deficiency, your red blood cells grow so large (macrocytic anemia) that they get stuck in your bone marrow and cannot enter the bloodstream to carry oxygen.
What is Vitamin B12 Deficiency?
To put it simply, Vitamin B12 Deficiency occurs when your body does not have enough of this essential vitamin to keep your blood cells healthy and your nervous system running smoothly. The Vitamin B12 Deficiency meaning goes beyond just “low vitamins”; it means your body is struggling to build the basic building blocks of life (DNA).
When you have a Vitamin B12 Deficiency, your nerves lose their insulation, similar to a frayed electrical wire. This leads to the various signs of Vitamin B12 Deficiency that doctors look for during a check-up. For a heart patient, this deficiency is particularly dangerous because it makes the heart work harder to pump blood that is poor in oxygen.
Why Vitamin B12 Deficiency Happens
Many patients ask, why Vitamin B12 Deficiency happens even if they eat a healthy diet. The answer usually lies in a process called absorption. Your stomach produces a special protein called “Intrinsic Factor.” Think of this protein as a “key” that unlocks B12 from your food. If your stomach is inflamed or if you are taking certain medications for acid reflux, your body cannot produce this key.
This leads to malabsorption B12 deficiency, where the vitamin is present in your food but cannot get into your blood. This is especially common in patients with metabolic disorders who may have gut problems and B12 deficiency issues due to long-term medication use or age-related changes in the digestive tract.
How Does the Body Absorb Vitamin B12?
Vitamin B12 absorption is a complex, multi-step biological process. Unlike many other vitamins, B12 cannot be absorbed directly from food without specific digestive support. Proper stomach and intestinal function are essential for this process.
First, when you consume foods containing Vitamin B12—such as dairy products, eggs, fish, or meat—the vitamin is tightly bound to proteins in that food. Inside the stomach, hydrochloric acid (HCl) and digestive enzymes break down these proteins, releasing free Vitamin B12. If stomach acid production is low—due to aging, long-term antacid use, or gastric disorders—this release step may be impaired.
Next, the freed Vitamin B12 attaches to a specialized protein called intrinsic factor. Intrinsic factor is produced by parietal cells in the lining of the stomach. This binding is crucial because Vitamin B12 cannot be efficiently absorbed without intrinsic factor.
Finally, the Vitamin B12–intrinsic factor complex travels to the last part of the small intestine (the ileum). There, specific receptors recognize this complex and allow B12 to be absorbed into the bloodstream.
This explains why individuals with intrinsic factor deficiency (such as in pernicious anemia) or intestinal disorders may develop Vitamin B12 deficiency—even if their dietary intake appears adequate.
Causes of Vitamin B12 Deficiency
Vitamin B12 deficiency develops either due to inadequate intake or impaired absorption. Since B12 absorption depends on proper stomach acid, intrinsic factor, and intestinal health, any disruption in this pathway can lead to deficiency.
Major Causes
-
Inadequate Dietary Intake
Individuals who consume very little or no animal-based foods (such as meat, fish, eggs, or dairy) may not get sufficient Vitamin B12. Long-term lack of fortified foods or supplements can gradually deplete body stores. -
Chronic Gastritis (Stomach Inflammation)
Persistent inflammation of the stomach lining can reduce the production of hydrochloric acid. Adequate stomach acid is necessary to release Vitamin B12 from food proteins, making gastritis a common contributor to deficiency. -
Pernicious Anemia
This autoimmune condition damages stomach cells responsible for producing intrinsic factor. Without intrinsic factor, Vitamin B12 cannot be absorbed efficiently in the small intestine. -
Intestinal Disorders (e.g., Crohn’s Disease, Celiac Disease)
Conditions affecting the small intestine, particularly the ileum, interfere with the final absorption step of Vitamin B12. -
Gastrointestinal Surgeries (e.g., Gastric Bypass)
Surgical procedures involving the stomach or small intestine may reduce acid production, intrinsic factor secretion, or the absorptive surface area — all of which are critical for B12 uptake. -
Chronic Alcohol Use
Long-term alcohol consumption can damage the stomach lining and intestinal cells, impairing both nutrient release and absorption. -
MTHFR Gene Mutation
Certain genetic variations affect how Vitamin B12 is metabolized at the cellular level. Individuals with this mutation may require higher doses or methylated forms of B12 for optimal function. -
Transcobalamin II Deficiency (Rare Genetic Disorder)
This uncommon inherited condition prevents proper transport of Vitamin B12 in the bloodstream, limiting its availability to body tissues.
Risk Factors for Vitamin B12 Deficiency
You may be at increased risk if you have one or more of the following:
-
Age above 75 years
Aging is associated with reduced stomach acid production and decreased absorption efficiency. -
Digestive System Disorders
Any chronic gastrointestinal disease can interfere with nutrient absorption, including Vitamin B12. -
Vegan or Strict Vegetarian Diet
Since Vitamin B12 is naturally found in animal-derived foods, individuals avoiding these foods must rely on fortified products or supplements. -
Long-Term Use of Certain Medications
Drugs such as metformin, proton pump inhibitors (PPIs), H2 blockers, and oral contraceptive pills may lower Vitamin B12 levels over time. -
Autoimmune Conditions (e.g., Sjögren’s Syndrome)
Autoimmune disorders may affect gastric function and increase the likelihood of deficiency. -
Excessive Alcohol Intake
Chronic alcohol exposure can impair both digestion and nutrient absorption.
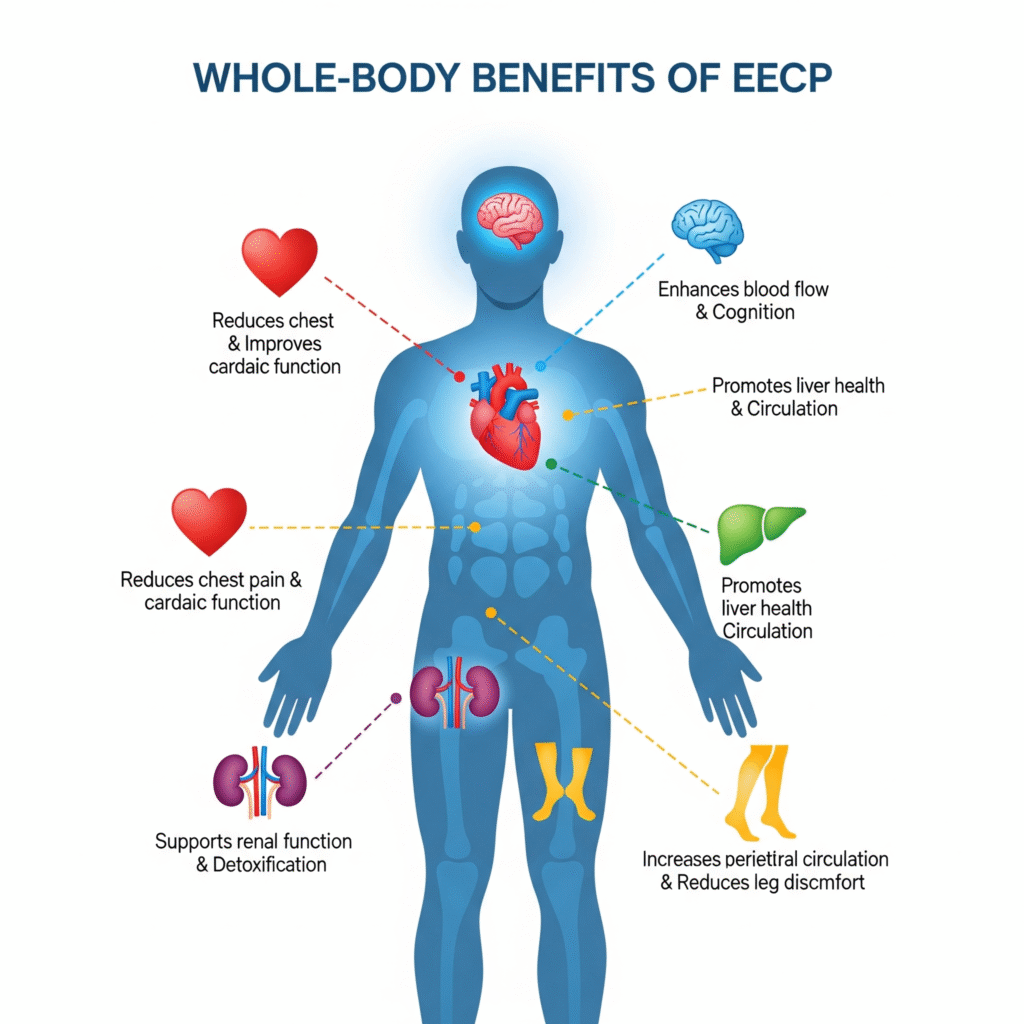
Signs of Vitamin B12 Deficiency
Recognizing the signs of Vitamin B12 Deficiency early can prevent permanent damage. Patients often ignore these signs, thinking they are just “getting older.” However, if you notice a persistent change in your energy or mood, it might be a Vitamin B12 Deficiency manifesting in your system.
One of the first signs is a change in the tongue, which may become swollen, red, and smooth. This is often accompanied by a loss of taste. For heart patients, a high heart rate or palpitations can also be among the early signs of Vitamin B12 Deficiency.
Vitamin B12 Deficiency Symptoms
The Vitamin B12 Deficiency symptoms can be split into physical and mental categories. In the early stages, you might experience a mild Vitamin B12 Deficiency, which feels like general sluggishness. However, if left untreated, it progresses into a severe Vitamin B12 Deficiency, which can be life-threatening.
Common physical Vitamin B12 Deficiency symptoms include:
- Extreme tiredness and lethargy.
- A “pins and needles” feeling in the limbs.
- Shortness of breath.
- A pale yellow tinge to the skin.
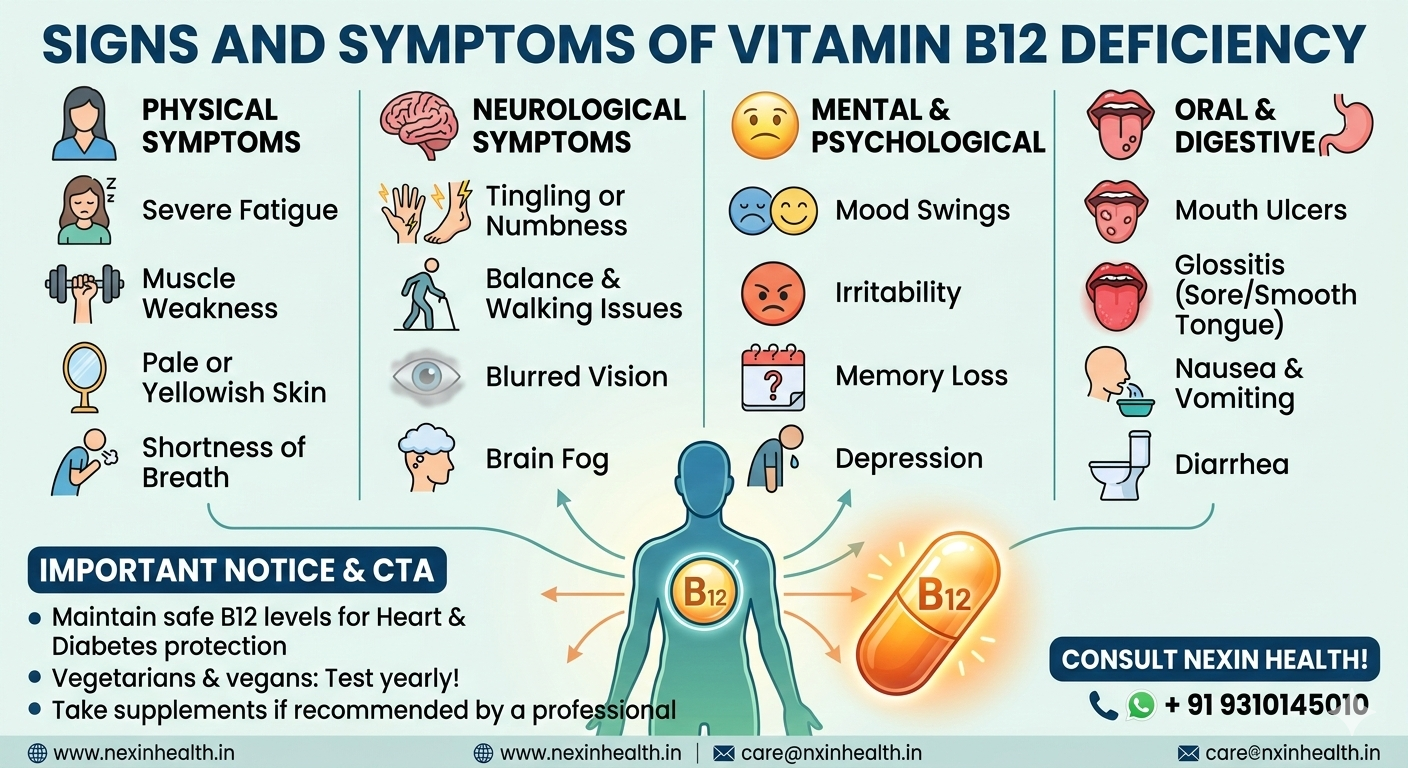
Vitamin B12 Deficiency Symptoms in Women
Research shows that Vitamin B12 Deficiency symptoms in women can often be confused with thyroid issues or menopause. Women may experience severe mood swings, irritability, and even postpartum depression linked to low B12 levels.
Furthermore, Vitamin B12 Deficiency in women can lead to temporary infertility or complications during pregnancy. If a woman is breastfeeding and has a Vitamin B12 Deficiency, her infant may also suffer from growth delays and developmental issues.
Vitamin B12 Deficiency Symptoms in Men
On the other hand, Vitamin B12 Deficiency symptoms in men often revolve around physical stamina and mental health. Men might notice a significant drop in their exercise tolerance.
In many cases, Vitamin B12 Deficiency in men is linked to erectile dysfunction because the nerves responsible for blood flow are not functioning correctly. Recognizing these Vitamin B12 Deficiency symptoms early can help men regain their vitality and heart health.
Vitamin B12 Deficiency Fatigue
One of the most reported issues is Vitamin B12 Deficiency fatigue. This is not your typical “tiredness” after a long day. It is a deep, bone-weary exhaustion that does not go away with rest.
This happens because your body cannot produce enough red blood cells to carry oxygen to your brain and muscles. This weakness due to B12 deficiency makes even simple tasks, like climbing a flight of stairs, feel like running a marathon. For a heart patient, this fatigue puts extra strain on a heart that is already struggling.
Neurological Symptoms of B12 Deficiency
B12 is the “protector” of your nervous system. Without it, the “wires” in your brain and spine begin to short-circuit. The neurological symptoms of B12 deficiency are often the most frightening for patients.
These symptoms include:
- Tingling in hands and feet B12: This feels like electricity or “ants crawling” on your skin.
- Memory loss Vitamin B12: You may find it hard to remember names, dates, or where you put your keys.
- Confusion: A general feeling of “brain fog” where you cannot think clearly.
- Balance Issues: A severe Vitamin B12 Deficiency can make you feel unsteady on your feet, increasing the risk of falls in the elderly.
Low Hemoglobin and B12 Deficiency
There is a direct link between low hemoglobin and B12 deficiency. Hemoglobin is the protein in your red blood cells that carries oxygen. When you have a Vitamin B12 Deficiency, your body struggles to make these cells.
This leads to a specific type of blood disorder called megaloblastic anemia. In this condition, the cells are too big and too few. Another related condition is macrocytic anemia, where the average size of the red blood cells (MCV) is much higher than normal. Both conditions result in your organs being starved of the oxygen they need to function.
Vitamin B12 Deficiency in Adults
As we navigate middle age, Vitamin B12 Deficiency in adults becomes more common due to lifestyle changes. Adults with metabolic syndrome or high blood pressure are often on multiple medications that can interfere with B12 levels.
If you are an adult managing diabetes, a Vitamin B12 Deficiency can worsen nerve pain (neuropathy), making it hard to tell if your symptoms are from high blood sugar or low vitamins. Regular screening for Vitamin B12 Deficiency is essential for anyone over the age of 40.
Vitamin B12 Deficiency in Elderly
The group most at risk is the elderly. Vitamin B12 Deficiency in elderly populations is often caused by “atrophic gastritis,” a condition where the stomach lining thins out as we age.
When an elderly person shows signs of confusion or memory loss Vitamin B12, family members often fear Alzheimer’s disease. However, many times, it is simply a chronic Vitamin B12 Deficiency that can be reversed with the right treatment. Keeping B12 at safe levels is a key part of healthy aging and heart protection.
Mild Vitamin B12 Deficiency vs. Severe Vitamin B12 Deficiency
It is important to understand the spectrum of this condition. A mild Vitamin B12 Deficiency might only cause slight fatigue or a bit of irritability. You might notice your heart racing a bit faster during a walk.
However, a severe Vitamin B12 Deficiency is a medical emergency. It can lead to permanent nerve damage, vision loss, and even psychiatric issues like paranoia or hallucinations. If you have been living with a long term Vitamin B12 Deficiency, the damage to your spinal cord can become irreversible. This is why early testing for Vitamin B12 Deficiency is so important.
Chronic Vitamin B12 Deficiency and Heart Health
For our heart patients, chronic Vitamin B12 Deficiency is a major concern. When B12 is low, a substance called homocysteine builds up in the blood. High homocysteine is like “sandpaper” inside your arteries; it creates tiny scratches that allow cholesterol to build up faster.
This means that even if your cholesterol is low, a Vitamin B12 Deficiency can still put you at risk for a heart attack. Managing your B12 is just as important as managing your blood pressure or blood sugar.
Comparison Table: Treatment Options for Vitamin B12 Deficiency
| Treatment Method | Best For | Speed of Recovery | Absorption Level |
| B12 Injections | Severe Vitamin B12 Deficiency | Very Fast | 100% (Bypasses gut) |
| Oral Supplements | Mild Vitamin B12 Deficiency | Slow to Moderate | Low (Depends on gut) |
| Sublingual (Drops) | Vitamin B12 Deficiency in Adults | Moderate | High (Absorbs via mouth) |
| Dietary Changes | Prevention of signs of Vitamin B12 Deficiency | Very Slow | Varies by food type |
| Nasal Sprays | Maintenance of safe levels | Moderate | Good |
Safe Levels and Diagnosis
How do you know if you have a Vitamin B12 Deficiency? A simple blood test can tell you. Generally, doctors look for the following ranges:
- Normal: Above 300 pg/mL.
- Borderline: 200 to 300 pg/mL (This is where mild Vitamin B12 Deficiency starts).
- Deficient: Below 200 pg/mL (This indicates a severe Vitamin B12 Deficiency).
However, many experts believe that for heart and diabetes patients, the “safe” level should be closer to 500 pg/mL to ensure optimal nerve and artery protection. If your levels are borderline, your doctor may check your MMA (Methylmalonic Acid) levels to confirm if a Vitamin B12 Deficiency is affecting your cells.
The Conventional Approach to Vitamin B12 Deficiency
The conventional medical approach to treating Vitamin B12 Deficiency usually involves high-dose supplements or “loading doses” of injections. If you have malabsorption B12 deficiency, your doctor will likely prescribe weekly shots for a month, followed by monthly shots for life.
While this solves the vitamin level, it often doesn’t address the underlying gut problems and B12 deficiency causes. An integrated approach that looks at your heart health, diet, and lifestyle is much more effective for long-term wellness.
Why Vitamin B12 is Crucial for Diabetic Patients
If you have diabetes, you are likely already worried about your nerves and your heart. A Vitamin B12 Deficiency acts as a “double whammy.” Diabetic neuropathy (nerve pain in the feet) feels almost exactly like the tingling in hands and feet B12 deficiency causes.
If you don’t treat the Vitamin B12 Deficiency, your diabetes medications might not be enough to stop the nerve pain. Clinical trials suggest that B12 helps in the regeneration of nerve fibers, making it a critical part of metabolic disorder management.
Vitamin B12 for Heart Disease Prevention
Can B12 prevent heart disease? While it is not a “magic pill,” maintaining safe levels of B12 ensures that your blood stays thin and your arteries stay smooth. By preventing megaloblastic anemia, you ensure that your heart doesn’t have to pump twice as fast to move oxygen around.
When we look at the Statistics of Vitamin B12 Deficiency, we see that patients who correct their levels often report better exercise capacity and lower stress levels. This makes Vitamin B12 Deficiency management a core pillar of preventive cardiology.
Vitamin B12 Sources for Vegetarians
While Vitamin B12 is predominantly found in animal products, vegetarians can optimize their intake through specific fermented and cultured foods. These traditional sources leverage bacterial synthesis to provide this essential nutrient:
-
Dairy-Based: Curd (Yogurt) and Kefir are excellent staples; the fermentation process increases B12 bioavailability compared to plain milk.
-
Traditional Ferments: Ambali (a fermented millet drink) and Home Fermented Pickles (in brine, not just oil) are heritage methods for boosting gut health and B12 levels.
-
Plant-Based Power: Natto (fermented soybeans) and Sauerkraut (fermented cabbage) offer unique microbial profiles. Kombucha provides a refreshing, effervescent B12 boost.
-
Living Foods: Sprouts are dense in enzymes, and when part of a balanced diet, they support the healthy gut environment necessary for nutrient assimilation.
Consuming these varied sources daily ensures a natural, integrated approach to maintaining healthy nerve function and energy levels.
How Vitamin B12 Works in Your Body
To understand the benefits of Vitamin B12, you have to look at the microscopic level. B12 acts as a helper (co-enzyme) for two major reactions:
- DNA Production: It helps your body make the instructions for every new cell.
- Energy Production: It helps turn the fats and proteins you eat into actual fuel for your heart and muscles.
This is why Vitamin B12 Deficiency fatigue is so debilitating—your body literally cannot create energy at a cellular level.
Consult the Experts: NexIn Health
At NexIn Health, we understand that heart and spine health are deeply connected to your nutritional status. NexIn Health is a leader in treating heart and spine conditions using Non-Invasive Integrated Techniques. With over 14+ years of experience and having consulted more than 30,000 patients, we focus on finding the root cause of your lifestyle diseases. Whether it is managing a Vitamin B12 Deficiency to protect your heart or using advanced tech to heal your spine, we are here to help.
Contact Us Today:
- Phone & WhatsApp: +91 9310145010
- Website: www.nexinhealth.in
- Email: care@nxinhealth.in
Read More:
Complete Treatment Guide for Vitamin B12 Deficiency
Treating a Vitamin B12 Deficiency is a journey, not a one-time event. Depending on the severity, here is the complete guide to recovery:
Step 1: Identify the Cause
Is it a vegetarian Vitamin B12 Deficiency? Or is it due to alcohol and B12 deficiency? Knowing the cause helps decide if you need pills or shots.
Step 2: Replenish Stores
For a severe Vitamin B12 Deficiency, you need injections to bypass the gut. For mild Vitamin B12 Deficiency, sublingual drops or high-dose pills (1000mcg) are often enough.
Step 3: Heal the Gut
Address gut problems and B12 deficiency by improving your digestion. This might include taking probiotics or managing acid reflux without overusing PPI medications.
Step 4: Monitor and Maintain
Once you reach safe levels, don’t stop! Continue with a maintenance dose, especially if you have a chronic Vitamin B12 Deficiency due to age or autoimmune issues.
The Role of Diet in Managing Vitamin B12 Deficiency
While supplements are often necessary, food is your first line of defense. To prevent signs of Vitamin B12 Deficiency, include the following in your diet:
-
Clams and Liver: The highest natural sources.
-
Fish: Salmon and trout are excellent for heart health and B12.
-
Dairy: Milk, cheese, and yogurt provide B12 in an easy-to-absorb form.
-
Fortified Foods: For those with a vegetarian Vitamin B12 Deficiency, look for B12-fortified nutritional yeast or cereals.
Vitamin B12 Deficiency and Metabolic Disorders
Metabolic disorders like obesity and insulin resistance often lead to systemic inflammation. This inflammation makes Vitamin B12 Deficiency symptoms even worse. By correcting a Vitamin B12 Deficiency, you improve your body’s ability to process carbohydrates and fats.
This helps in weight management and improves overall energy levels, making it easier to stay active—the best medicine for any heart patient.
The Danger of Long Term Vitamin B12 Deficiency
We cannot stress enough the danger of a long term Vitamin B12 Deficiency. Unlike a cold or a flu, B12 issues do not just “go away.” The longer you wait, the higher the chance of neurological symptoms of B12 deficiency becoming permanent.
If you have been feeling weakness due to B12 deficiency for more than six months, it is time to seek professional help. Your heart and your brain depend on it.
Summary of Vitamin B12 Deficiency Management
In conclusion, Vitamin B12 Deficiency is a manageable but serious condition. From understanding why Vitamin B12 Deficiency happens to recognizing the Vitamin B12 Deficiency symptoms in women and men, being informed is your best tool.
Keep your levels at a safe level, watch for signs of Vitamin B12 Deficiency, and work with experts like NexIn Health to ensure your heart and nerves stay strong for years to come.
Frequently Asked Questions (FAQs) for Heart Patients
Que: Can Vitamin B12 Deficiency cause chest pain?
Ans: While it doesn’t directly cause a heart attack, the Vitamin B12 Deficiency fatigue and rapid heart rate caused by anemia can lead to chest discomfort or palpitations, making the heart work harder than it should.
Que: I take blood thinners; can I take B12 supplements?
Ans: Yes, B12 usually does not interact with blood thinners. In fact, maintaining safe levels of B12 helps keep your homocysteine low, which supports the health of your blood vessels.
Que: How does B12 help if I have high blood pressure?
Ans: B12 supports the health of the lining of your blood vessels (endothelium). By preventing chronic Vitamin B12 Deficiency, you help your arteries stay flexible, which is essential for managing blood pressure.
Que: Can a heart patient get B12 injections?
Ans: Yes, injections are often the fastest way to reverse a severe Vitamin B12 Deficiency. They are generally safe for heart patients and bypass any malabsorption B12 deficiency issues in the gut.
Que: Does Metformin cause Vitamin B12 Deficiency in everyone?
Ans: Not everyone, but it is very common. Clinical trials suggest that anyone on Metformin for more than a year should be tested for Vitamin B12 Deficiency annually to prevent nerve damage.
Que: Can B12 improve my heart’s pumping capacity?
Ans: If your heart is struggling due to megaloblastic anemia, then yes, treating the Vitamin B12 Deficiency will improve your oxygen levels and help your heart pump more efficiently.
Que: Is there a specific “heart-safe” type of B12?
Ans: Methylcobalamin is the “active” form of B12 and is often preferred for those with heart issues or metabolic disorders because it is easier for the body to use immediately.
Que: How long does it take to feel better after starting B12 treatment?
Ans: You might feel a boost in energy within a few days of an injection. However, for neurological symptoms of B12 deficiency like tingling or memory loss, it can take weeks or even months to see a full recovery.
Que: Can Vitamin B12 Deficiency cause high cholesterol?
Ans: No, but it causes high homocysteine. Both high cholesterol and high homocysteine work together to clog your arteries, so you must manage both to protect your heart.
Que: I am a vegetarian heart patient; how often should I test for B12?
Ans: Because of the high risk of vegetarian Vitamin B12 Deficiency, it is recommended to get tested at least twice a year to ensure your levels stay in the safe level range.