How Much Sugar Should You Eat In a Day: Have you ever counted how many teaspoons of sugar go into your morning chai? Or wondered why your post-meal mithai cravings feel impossible to control? With diabetes affecting over 77 million people in our country and heart disease rates climbing steadily, understanding daily sugar intake has become a critical health priority for every household.
Sugar undoubtedly enhances the flavors we love – from traditional sweets during festivals to the comfort of sweetened tea breaks. It provides quick energy for our demanding lifestyles, whether you’re managing household responsibilities, working long hours, or caring for elderly parents. However, our modern eating habits have led many families to consume far more sugar than our bodies can handle effectively.
The startling reality? Most people in our urban and semi-urban areas consume nearly three times the recommended amount of added sugar daily, often without realizing it. This excessive sugar consumption pattern reveals a hidden health crisis affecting millions of families across metropolitan cities, tier-2 towns, and even rural areas adopting processed food habits.
But here’s the encouraging news – understanding optimal daily sugar intake and implementing practical dietary changes can dramatically improve health outcomes for you and your loved ones, regardless of your current eating habits or family traditions.
Fact Sheet: Eye-Opening Sugar Statistics for Our Population
🔥 Did You Know These Shocking Sugar Facts About Our Eating Habits?
- The average urban dweller consumes 17 teaspoons of added sugar daily – equivalent to drinking nearly 3 bottles of sweetened lassi every single day!
- One serving of popular flavored dahi contains 9 grams of added sugar – that’s 40% of your recommended daily intake in just one small bowl.
- Traditional sweets during festivals can contain 15-25 grams of sugar per piece – a single gulab jamun or rasgulla exceeding half your daily sugar allowance.
- Packaged fruit juices marketed as healthy contain more sugar than cola – with some popular brands packing 8-10 teaspoons per 200ml serving.
- Sweetened beverages account for 50% of total added sugar intake – including sweetened chai, cold drinks, and packaged fruit drinks.
- Children under 2 years should consume absolutely zero added sugar – yet many families introduce sweet foods much earlier due to cultural practices.
- Home-cooked meals with traditional jaggery and sugar can exceed daily limits – especially when combined with processed snacks and beverages.
- Complex carbohydrates from millets and whole grains prevent blood sugar spikes – making traditional grains healthier choices than refined alternatives.
Understanding Recommended Daily Sugar Intake for Our Population
What Leading Health Organizations Recommend
The question of safe daily sugar consumption has been extensively researched by international health bodies, with recommendations that apply universally regardless of geographic location or cultural food preferences. These evidence-based guidelines provide a foundation for maintaining optimal health while enjoying traditional foods.
Global Dietary Guidelines recommend that adults limit added sugar intake to no more than 10% of total daily calories. For someone following a typical 2,000-calorie diet – common among working professionals and homemakers – this translates to approximately 12 teaspoons or 50 grams of added sugar daily.
However, heart health specialists worldwide take a stricter approach, suggesting adults consume no more than 6% of daily calories from added sugars. This conservative recommendation amounts to just 6-9 teaspoons (about 30 grams) of sugar daily for a 2,000-calorie diet – roughly equivalent to 2-3 pieces of traditional sweets.
Special Guidelines for Children and Teenagers
Children’s sugar consumption requires even more careful attention due to their developing bodies, smaller caloric needs, and vulnerability to establishing lifelong eating patterns. Pediatric nutrition experts provide clear recommendations:
Infants under 2 years old should receive absolutely no added sugars. Their digestive systems are still maturing, and early sugar exposure can program their taste preferences toward overly sweet foods throughout life.
Children and teenagers over 2 years old should limit added sugar intake to no more than 6 teaspoons (25 grams) per day. This restriction helps prevent childhood obesity, dental problems, and supports healthy growth during crucial developmental years.
These guidelines become particularly important during festivals and celebrations when children are typically offered numerous sweet treats by well-meaning relatives and family friends.
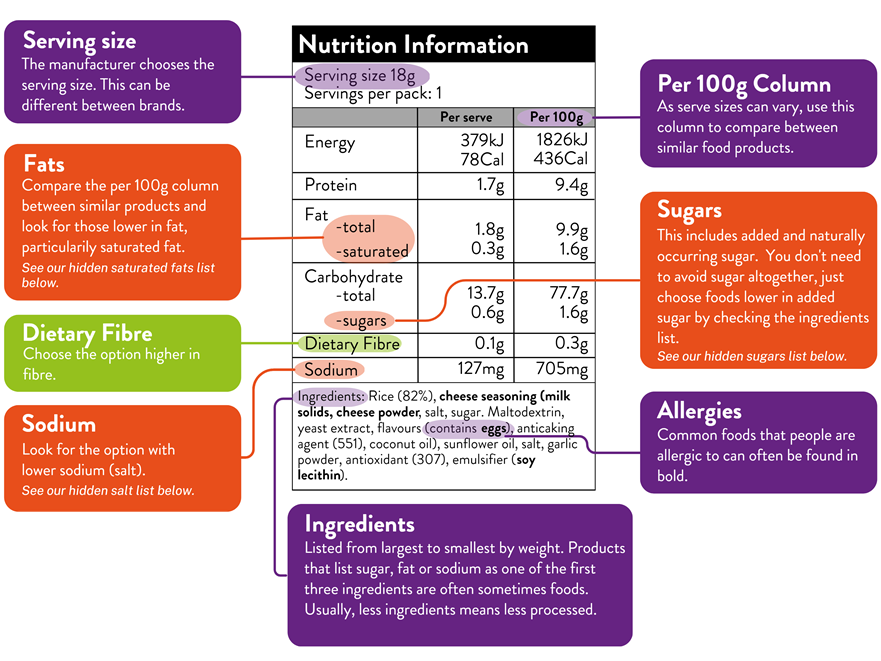
Decoding Food Labels: Understanding Natural vs Added Sugar Content
How to Read Nutrition Information on Packaged Foods
Understanding food labels empowers families to make informed choices about daily sugar consumption and helps identify hidden sugars in seemingly healthy products. Modern packaging provides detailed nutritional breakdowns that distinguish between beneficial and potentially harmful sugars.
Total Sugar represents the combined amount of natural and added sugars in the product. This includes naturally occurring sugars from ingredients like milk, fruits, or vegetables used in processing.
Added Sugars specifically indicates sweeteners that manufacturers have incorporated during production or that home cooks might add during preparation. This number will always equal or be less than the total sugar content listed.
For instance, a packaged lassi might show 15 grams of total sugar but only 5 grams of added sugar, indicating that 10 grams come from natural milk sugars while 5 grams represent processed sweeteners added for taste enhancement.
The Science Behind Natural vs Added Sugar Processing
Your body’s sugar metabolism reveals important differences between natural and processed sweeteners, with significant implications for blood sugar control and overall health. Understanding these differences helps explain why traditional whole foods generally support better health outcomes.
Natural sugars in whole foods come bundled with fiber, vitamins, minerals, and protective compounds. These complex carbohydrates contain multiple sugar molecules and require more digestive energy, resulting in gradual absorption and stable blood glucose levels.
Added sugars are simple carbohydrates that your body absorbs rapidly, causing sharp spikes in blood sugar levels. Without accompanying nutrients, these calories provide immediate energy but offer no additional health benefits.
The fiber content in natural sugar sources promotes beneficial short-chain fatty acid (SCFA) production during digestion. These helpful compounds support gut health by nourishing beneficial bacteria in your digestive system and improving overall intestinal function – particularly important for maintaining digestive wellness.
Health Consequences of Excessive Sugar Consumption
Understanding the Risks of High Daily Sugar Intake
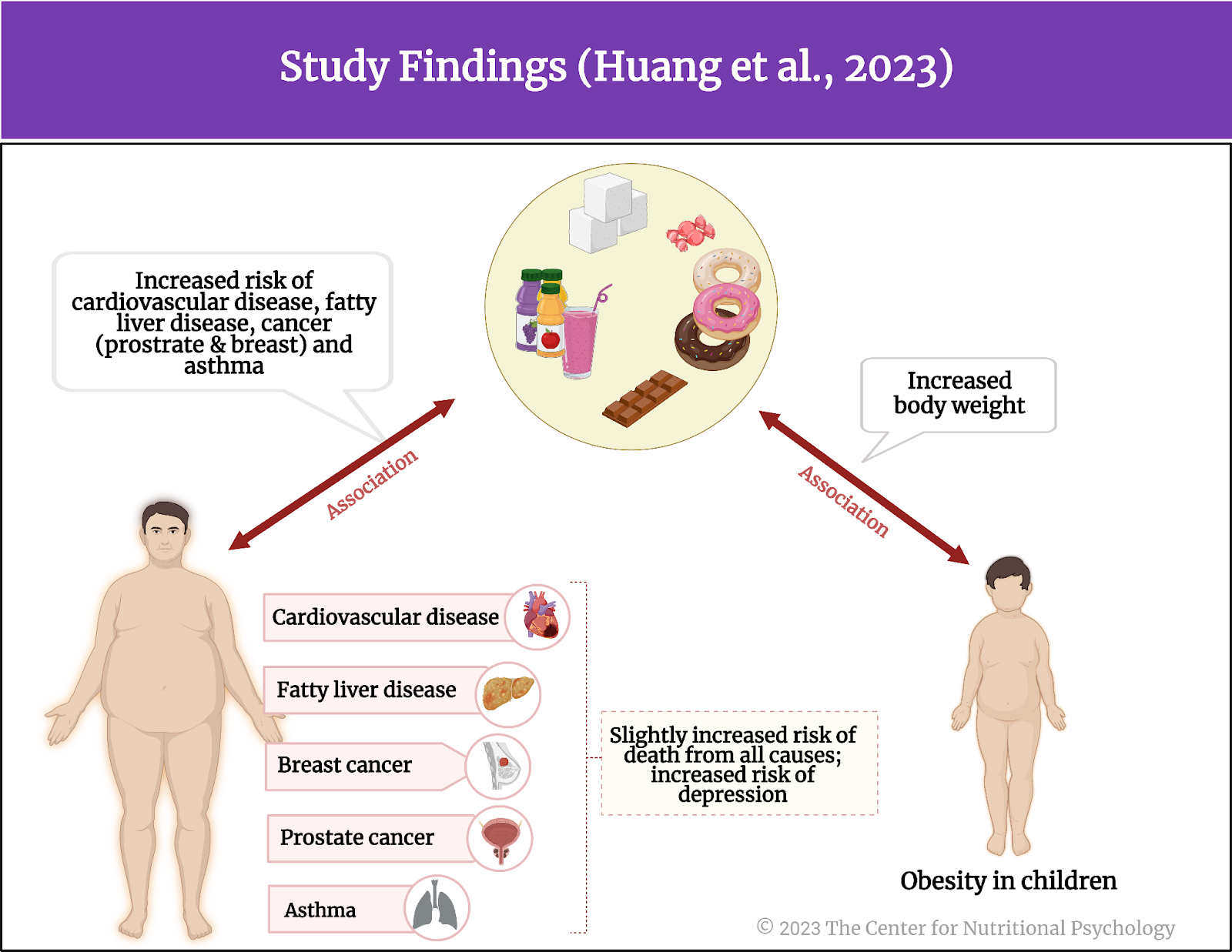
Consuming excessive sugar daily creates a cascade of health problems that extend far beyond simple weight gain. The relationship between high sugar consumption and chronic diseases has been extensively documented through population studies and clinical research conducted across diverse communities.
Excess calorie intake from sugar contributes to unwanted weight gain, as surplus calories convert to stored body fat regardless of their source. However, sugar calories pose particular challenges because they don’t trigger the same fullness signals as protein or healthy fats, leading to continued eating.
Chronic health conditions associated with high sugar intake include hypertension (high blood pressure), cardiovascular disease, sleep breathing disorders, joint problems, persistent pain conditions, and certain cancers. These conditions often develop gradually over years of excessive sugar consumption patterns.
Effect of Sugar on Health – NexIn Health
Read Research Paper:
Dental Health Impact of Sugar Consumption
The connection between sugar intake and dental problems represents one of the most well-established relationships in nutritional science. Sugar provides fuel for harmful oral bacteria, leading to acid production that gradually destroys tooth enamel and supporting structures.
Dental decay risk increases dramatically with higher added sugar consumption. Research consistently demonstrates that people consuming more than 10% of their calories from added sugars experience significantly more cavities, tooth loss, and gum disease.
Natural sugars in whole foods like milk and fresh fruits pose minimal dental health risks due to their accompanying protective nutrients. The calcium in dairy products actually helps strengthen tooth enamel, while fiber and water content in fruits help cleanse the mouth naturally during eating.
However, dried fruits and sticky sweets can be problematic because they adhere to tooth surfaces and concentrate sugars without the protective water content found in fresh alternatives. Traditional sweets like kheer, halwa, and laddu require careful oral hygiene afterward.
Cardiovascular Disease and Sugar Relationship
The strict sugar recommendations from heart health organizations stem from mounting evidence linking added sugar consumption with cardiovascular disease risk factors. While research continues evolving, several concerning patterns have emerged from population health studies.
Sugar-sweetened beverages demonstrate the strongest association with heart disease risk across multiple research investigations. Regular consumption of soft drinks, sweetened teas, energy drinks, and processed fruit drinks correlates with increased cardiovascular problems.
Research findings show mixed results regarding other forms of added sugar and heart disease development. Some studies reveal clear relationships, while others indicate more complex interactions involving overall dietary quality, physical activity levels, and genetic predisposition factors.
The observational nature of most nutrition research creates challenges in establishing direct cause-and-effect relationships. However, the weight of evidence suggests that limiting added sugar supports cardiovascular wellness as part of comprehensive healthy lifestyle practices.
Type 2 Diabetes Risk Factors and Sugar Consumption
The relationship between sugar intake and diabetes risk proves more complex than many people understand. While managing sugar consumption becomes crucial for people already diagnosed with diabetes, preventing the disease involves multiple lifestyle and hereditary factors.
Established diabetes risk factors include family history, sedentary lifestyle habits, age over 45 years, and excess body weight accumulation. Added sugar consumption alone is not considered a primary risk factor for developing type 2 diabetes.
Blood glucose management becomes critical once diabetes develops. People with diabetes must carefully monitor sugar intake to prevent dangerous blood glucose fluctuations that can lead to serious short-term and long-term complications.
Sugar-sweetened beverages represent the strongest dietary connection to diabetes risk according to prevention research. Diabetes specialists specifically recommend eliminating these drinks and choosing water, unsweetened tea, or other low-calorie alternatives whenever possible.
Non-Alcoholic Fatty Liver Disease (NAFLD) Connection
NAFLD represents one of the fastest-growing liver conditions, affecting millions of people who consume little or no alcohol. Emerging research suggests that certain types of added sugars may contribute significantly to this serious health problem.
Added fructose consumption, particularly from sugar-sweetened beverages and processed foods, shows strong associations with increased NAFLD risk in several population studies. High-fructose corn syrup, commonly used in packaged foods and drinks, raises particular concern among researchers.
Liver fat accumulation occurs when the liver cannot process all incoming fructose efficiently, converting excess sugar into stored fat within liver cells. Over time, this accumulation can trigger inflammation and progressive liver damage.
Multiple factors influence NAFLD development, including genetics, overall diet quality, exercise habits, and existing health conditions like type 2 diabetes. However, reducing sugar-sweetened beverage consumption appears to offer significant protective benefits.
Hidden Sugar Sources: Foods with Surprising Sugar Content
Beverages: The Primary Source of Added Sugar
Understanding where added sugars hide in daily food choices helps identify the most impactful dietary modifications for reducing total intake. Beverages consistently rank as the leading source of added sugars, contributing approximately 50% of total consumption across different age groups.
Common high-sugar beverages include carbonated soft drinks, packaged fruit drinks, sports and energy drinks, sweetened coffee beverages, flavored teas, and even some traditional drinks like sweetened buttermilk or flavored milk products.
Tea and coffee preparations can contain shocking amounts of added sugar, especially when prepared with multiple teaspoons of sugar or condensed milk. A large sweetened chai from popular outlets might contain 6-8 teaspoons of added sugar, nearly reaching entire daily limits in one serving.
Packaged fruit juices often contain more sugar than traditional soft drinks, despite marketing claims about natural ingredients and health benefits. Many popular brands pack 8-12 teaspoons of sugar per standard serving.
Unexpected Food Sources of Added Sugar
Many everyday foods contain hidden sugars that surprise health-conscious consumers. These unexpected sources often contribute substantially to daily sugar intake without providing the satisfaction or awareness associated with obvious sweet treats.
Bread and bakery products can contribute significantly to daily sugar intake, as manufacturers use sugar as a preservative and flavor enhancer. Traditional Indian breads like commercially produced rotis, naans, and packaged bread varieties often contain added sugars.
Breakfast cereals and health bars frequently market themselves as nutritious options while containing substantial amounts of added sugar. Some popular cereals contain more sugar per serving than traditional sweets, despite health-focused packaging and marketing claims.
Flavored dairy products including sweetened yogurt, flavored milk, and processed cheese products often contain 6-15 grams of added sugar per serving. These products trade on dairy’s healthy reputation while delivering significant sugar loads.
Packaged sauces and condiments can add considerable sugar to otherwise healthy home-cooked meals. Tomato ketchup, sweet and sour sauces, salad dressings, and even some curry bases contain sugar or high-fructose corn syrup among primary ingredients.
Traditional sweets and festival foods obviously contain high sugar levels, but the quantities often exceed expectations. A single piece of popular sweets like gulab jamun, jalebi, or barfi can contain 15-25 grams of sugar – approaching or exceeding entire daily recommendations.
Practical Strategies for Reducing Daily Sugar Intake
Making Smart Beverage Choices
Since beverages contribute half of total added sugar consumption, modifying drink choices offers the greatest opportunity for meaningful reduction while maintaining satisfaction and cultural food enjoyment practices.
Gradual reduction approaches prove more successful than dramatic changes for long-term habit modification. Start by reducing sugar in daily tea or coffee by half a teaspoon weekly, or dilute fruit juices with plain or sparkling water to maintain familiar flavors.
Healthy beverage alternatives include plain water (room temperature or chilled), unsweetened tea varieties (green, black, herbal), fresh lime water with minimal sweetener, buttermilk without added sugar, and coconut water for natural electrolyte replenishment.
Traditional drink modifications can maintain cultural preferences while reducing sugar content. Prepare masala chai with less sugar and more spices, make fresh fruit-infused water, or enjoy traditional drinks like jaljeera with reduced sweetener and increased spice content.
Smart Food Preparation and Shopping Strategies
Whole food snack alternatives provide natural sweetness along with beneficial nutrients. Choose fresh seasonal fruits, nuts and seeds, roasted chickpeas, vegetable sticks with homemade chutneys, or plain yogurt with fresh fruit instead of processed snacks.
Home cooking control allows complete management of sugar content in family meals. Purchase unsweetened products and add controlled amounts of natural sweeteners like jaggery, honey, or fresh fruit to achieve desired taste levels.
Balanced meal planning helps prevent sugar cravings by maintaining stable blood sugar throughout the day. Include protein sources, healthy fats, and fiber-rich foods in each meal to promote satiety and reduce evening sweet cravings.
Festival and celebration strategies help maintain social connections while managing sugar intake. Prepare smaller portions of traditional sweets, share treats with extended family and neighbors, or create modified versions using less sugar and more nuts, seeds, or fruit.
Reading Labels and Making Informed Purchasing Decisions
Ingredient awareness helps identify hidden sugars appearing under various names on packaged foods. Look for terms like high-fructose corn syrup, cane sugar, invert sugar, glucose syrup, and concentrated fruit juices in ingredient lists.
Prioritizing minimally processed foods when shopping provides better control over sugar content. Choose whole grains over refined products, fresh fruits over canned varieties, and plain dairy products that can be customized with natural sweeteners at home.
Portion control strategies allow occasional enjoyment of favorite sweet foods without exceeding daily recommendations. When choosing high-sugar treats, eat smaller portions mindfully and savor the experience rather than consuming unconsciously.
The Benefits of Reducing Sugar Consumption
Immediate Health Improvements
Energy level stabilization occurs within days of reducing added sugar intake. Instead of experiencing energy peaks and crashes throughout the day, you’ll maintain more consistent energy levels that support sustained productivity and better mood regulation.
Improved sleep quality often follows sugar reduction efforts, as stable blood sugar levels support better sleep patterns and reduce nighttime awakenings. Many people report falling asleep more easily and waking more refreshed.
Enhanced taste sensitivity develops over several weeks as your palate adjusts to lower sweetness levels. Natural flavors in foods become more pronounced and satisfying, and you’ll discover new appreciation for subtle tastes in traditional dishes.
Long-term Health Benefits
Reduced chronic disease risk includes lower probability of developing type 2 diabetes, cardiovascular disease, and certain cancers associated with excessive sugar consumption patterns documented in long-term population studies.
Better dental health results from decreased cavity-causing bacteria in your mouth, leading to fewer dental problems, reduced treatment needs, and lower dental care costs over time.
Weight management support becomes more achievable as you eliminate empty calories from added sugars and experience reduced cravings for high-calorie processed foods that often trigger overeating episodes.
Improved digestive health develops as your gut bacteria composition shifts toward beneficial strains that thrive on complex carbohydrates rather than simple sugars, supporting better nutrient absorption and immune function.
Creating a Sustainable Low-Sugar Lifestyle
Building Healthy Habits Gradually
Incremental changes prove more successful than dramatic dietary overhauls that feel overwhelming or unsustainable. Focus on one modification at a time, such as reducing sugar in beverages before addressing sweet snacks or festival foods.
Mindful eating practices help distinguish true hunger from sugar cravings, allowing conscious decisions about when and how much sugar to consume. This awareness particularly helps during social situations and cultural celebrations.
Family support systems enhance success in maintaining reduced sugar intake across all household members. Involve family members in meal planning, shopping decisions, and preparation of healthier alternatives to traditional high-sugar foods.
Meal Planning and Preparation Strategies
Weekly meal planning ensures healthy, low-sugar options remain readily available when hunger strikes or time pressures increase. Prepare cut vegetables, portioned nuts, washed fruits, and homemade snacks for convenient healthy choices.
Batch cooking techniques allow preparation of large quantities of healthy, low-sugar meals that can be portioned and stored for busy periods when processed food convenience might otherwise win.
Emergency snack preparation prevents impulsive high-sugar food choices during extremely hungry moments or when time constraints limit thoughtful food selection. Keep healthy options easily accessible in multiple locations.
Frequently Asked Questions: How Much Sugar Should You Eat In a Day
Que: How much sugar per day is safe for someone managing diabetes?
Ans: People with diabetes should work closely with their healthcare provider to determine appropriate sugar intake based on their specific condition, medications, and blood sugar patterns. Generally, the same guidelines apply (6-10% of total calories), but individual responses vary significantly. Focus on complex carbohydrates from traditional whole grains and monitor blood glucose levels when consuming any sugars, including natural sources.
Que: Can I eat unlimited natural sugars from fruits since they provide vitamins and minerals?
Ans: While fruits offer beneficial nutrients, they still contain calories and natural sugars that count toward total daily intake. Most people can enjoy 2-4 servings of whole fruits daily without health concerns. However, fruit juices and dried fruits should be limited as they concentrate sugars without the beneficial fiber found in whole fruits. Choose seasonal, locally available fruits for optimal nutrition and cost-effectiveness.
Que: Is jaggery healthier than white sugar for daily cooking and tea preparation?
Ans: Jaggery contains small amounts of iron, potassium, and other minerals that white sugar lacks, but both affect blood sugar levels similarly. The key is moderation – use jaggery sparingly and count it toward your daily added sugar limit. Organic, unprocessed jaggery may provide slightly more nutrients than refined varieties, but portion control remains essential.
Que: How quickly will I notice health benefits after reducing sugar intake?
Ans: Many people experience improved energy levels and reduced cravings within 1-2 weeks of cutting added sugar consumption. Weight changes and improved blood markers may take 4-8 weeks to become apparent. Long-term benefits like reduced chronic disease risk develop over months and years of sustained healthy eating patterns.
Que: What should I do about sugar consumption during festivals and family celebrations?
Ans: Enjoy traditional sweets in smaller portions, focus on sharing treats with extended family and friends, prepare homemade versions with reduced sugar content, and balance celebration days with extra attention to sugar intake for several days afterward. Remember that occasional indulgence won’t derail overall health if your daily habits remain consistent.
Que: Are natural sweeteners like honey and dates better choices for children?
Ans: Natural sweeteners like honey (after age 1), dates, and pure maple syrup contain beneficial compounds that white sugar lacks, but all should be used sparingly in children’s diets. These alternatives still contribute to total sugar intake and can promote sweet taste preferences. Focus on offering naturally sweet foods like fruits and limit all added sweeteners regardless of source.
Que: How do I manage sugar cravings while reducing overall intake?
Ans: Eat balanced meals with protein, healthy fats, and fiber to stabilize blood sugar and reduce cravings. When cravings occur, try drinking water, eating fresh fruit, taking a short walk, or practicing deep breathing. Cravings typically diminish significantly after 2-3 weeks of consistent lower sugar consumption as taste preferences adapt.
Que: Should people with family history of diabetes avoid all sugars completely?
Ans: Family history of diabetes increases risk but doesn’t require complete sugar avoidance. Focus on maintaining healthy body weight, exercising regularly, and limiting added sugars while including natural sugars from whole foods in moderation. Regular health screenings help detect any blood sugar changes early when interventions are most effective.
Que: What should I do if I accidentally consume too much sugar in one day?
Ans: Don’t panic or attempt to compensate by severely restricting food intake the following day. Simply return to normal healthy eating patterns and drink plenty of water. Consider taking a walk to help your body process excess glucose. Focus on learning from the experience to prevent similar situations in the future.
Que: How does stress affect sugar cravings and consumption patterns?
Ans: Stress increases cortisol production, which triggers cravings for high-sugar, high-fat comfort foods. Chronic stress makes resisting these cravings much more difficult. Managing stress through regular exercise, meditation, adequate sleep, and relaxation practices helps reduce sugar cravings naturally while supporting overall health.
Que: Is it realistic to completely eliminate added sugars from my family’s diet?
Ans: Complete elimination of added sugars is unnecessary for most families and may create social difficulties during celebrations and cultural events. Focus on reducing added sugars to recommended levels rather than complete elimination. This approach proves more sustainable long-term and allows for occasional treats within an overall healthy eating pattern.
Que: How do I make healthy choices when eating at restaurants or social gatherings?
Ans: Ask for dressings and sauces on the side, choose grilled or steamed preparations over sweet and glazed dishes, request fresh fruit or plain yogurt for dessert, and opt for unsweetened beverages. Don’t hesitate to ask about sugar content in dishes – most restaurants can provide basic nutritional information. Plan ahead by eating a small, balanced snack before social events to avoid arriving overly hungry.
About the Author
Mr. Vivek Singh Sengar is a renowned clinical nutritionist, EECP trainer, and researcher with extensive expertise in treating lifestyle disorders and cardiovascular diseases. As the founder of FIT MY HEART and consultant at NEXIN HEALTH and MD CITY Hospital Noida, he has successfully treated over 25,000 heart and diabetes patients across the globe.
Mr. Sengar’s unique approach combines evidence-based EECP therapy with comprehensive nutritional interventions and lifestyle modifications. His research contributions have advanced understanding of EECP applications in various cardiovascular conditions. Through his practice at www.viveksengar.in, he continues to provide cutting-edge cardiac care while training the next generation of EECP practitioners.
His expertise spans clinical nutrition, cardiovascular disease management, diabetes care, and non-invasive cardiac therapies. Mr. Sengar’s commitment to patient-centered care and evidence-based medicine has established him as a leading authority in EECP therapy and lifestyle disease management.
💬 Need Expert Guidance for Your Health?
🌿 NexIn Health is India’s Leading Integrated Wellness Center, specializing in:
-
Non-Surgical Heart Disease Treatments
-
Diabetes Reversal Programs
-
Pain Management
-
Obesity & Fatty Liver Management
-
Women’s Hormonal Health (PCOS, Menopause, etc.)
With a team of 25+ wellness coaches, doctors, clinical nutritionists, and researchers, and over 30 centers globally, NexIn Health combines modern science with natural, non-invasive healing methods — empowering patients to reclaim their health without surgery or lifelong medications.
🔗 Visit NexIn Health: www.nexinhealth.in
📞 Call or WhatsApp: +91 9310 14 5010
📩 Email: care@nexinhealth.in
✅ Whether you’re seeking a second opinion or want to reverse your health condition naturally — take the first step towards healing today.
Your health transformation begins with the right expert.
Connect Now. Live Better.
Also Read: Ayurverdic Heart Blockage Treatment
